To Issue 141
Citation: Krummenacher F, Müller P, “Designing Effective and Engaging Digital Solutions to Drive Adherence”. ONdrugDelivery, Issue 141 (Dec 2022), pp 10–14.
Florian Krummenacher and Philippe Müller discuss the effectiveness of combining connected injection devices with digital solutions to drive therapy outcomes.
“Adherence to treatment regimens can be a challenge for AD patients.”
Laura sits at home in the heat of summer. Her friends are at the local pool, but Laura has not joined them today. In fact, she hasn’t joined them all summer. Her skin itches and her rashes are visible; this makes her feel ashamed and she doesn’t want anyone to see it. All the while, the anti-inflammatory injectable drug she was prescribed to treat her condition sits unused in her fridge. Laura doesn’t like to inject herself and doesn’t even want to think about having to do it. She knows that the medication will probably help, and that not taking her medication will only make things worse, but she can’t help it. Her fear and hesitancy take over and dictate her inaction.
While a fictitious example, this situation is all too often the reality for people living with chronic skin diseases such as atopic dermatitis (AD) and psoriasis. AD is a chronic inflammatory skin disease that affects about one in every ten people worldwide and up to one in five children.1 It is thought to be caused by a combination of genetic and environmental factors, causing the immune system to overreact, leaving the skin dry and prone to rashes. While the disease typically begins in early childhood, it can become a lifelong burden with flare-ups well into adulthood. The condition can be highly distressing for sufferers and is often stigmatised. It can also have a significant negative impact on day-to-day life, both personal and professional, as sufferers may find it difficult to wear certain clothing and are often affected by itching, which can lead to insomnia, anxiety and depression.2
NEED FOR A MULTIFACETED APPROACH
Depending on the severity of the disease, the current standard of care may range from behavioural changes to tailored medication. The latter includes both topical steroids and biologics, such as anti-inflammatory drugs, which are often injected subcutaneously by the patients themselves. Besides medication, lifestyle choices can have a big impact on the severity of symptoms and disease progression, affecting the patient’s experience. Avoiding certain situations that might trigger a flare-up of the disease is one of the measures that can help to manage the disease. Ensuring that the skin is appropriately hydrated can also help to reduce symptoms. Eating a healthy diet, limiting stress and maintaining good sleep hygiene are other important factors.
As with many chronic conditions, adherence to treatment regimens can be a challenge for patients, who can often feel isolated and unsupported in their disease journey. The reasons for these feelings are often varied, as outlined in the example above, and this can have an adverse effect on the patient’s health outcomes.3
Injection device manufacturer Ypsomed supports patients by making self-medication with injectable biologics as simple as possible using pens and autoinjectors. To better embed self-injection in broader therapy management, Ypsomed has joined forces with digital therapeutics developer Sidekick Health (Reykjavík, Iceland). The two companies are jointly developing a module on self-injection that will be part of Sidekick’s existing digital therapeutics platform, which is already available for AD patients in several countries, including the UK, Belgium and Finland (Figure 1).
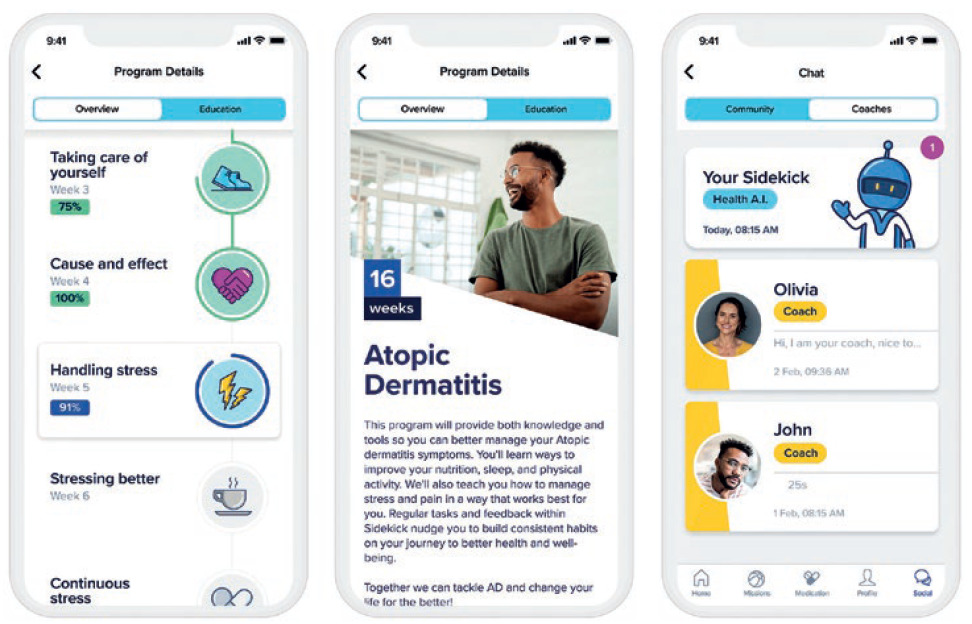
Figure 1: The Sidekick app offers comprehensive support for AD patients.
EFFICACY OF A DIGITAL SOLUTION
Living with AD and managing the therapy is a complex challenge and requires a lot of active engagement, know-how and resilience from patients. Digital solutions that complement the pharmaceutical drug have shown to provide significant value to patients, caregivers and healthcare professionals by improving medication adherence, quality of life and therapy outcomes. There are several modes of action for a digital therapeutics solution – for example, using neuro behavioural techniques to improve patients’ self-management capabilities, personalised disease-specific knowledge, simplifying treatment scheduling and management of symptoms and side effects, tracking medication intakes and supporting the adoption of a healthier lifestyle (Figure 2).
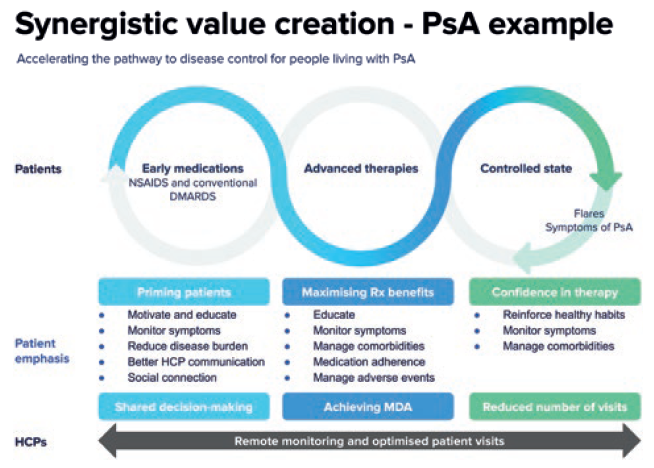
Figure 2: The patient journey for psoriatic arthritis (PsA) patients.
“A key success factor of the app lies in its ability to be personalised to the individual patient.”
In a recently published study in the Dermatology and Therapy Journal, Sidekick evaluated the clinical efficacy of its digital therapeutics programme in patients with AD. For patients enrolled in the six-week digital programme, it reported an average reduction in AD severity of 46%, higher medication adherence and improved quality of life.4 The programme included the following key functionalities provided to the users as support tools or missions – patient education, medication reminders, symptom tracking, stress reduction and sleep improvement to overall facilitate behaviour change toward self-efficacy.
Besides the improvements in therapy outcomes, Sidekick found strong engagement and retention results in the study. Patient retention to the digital therapeutics programme was 95.3% at completion of the six-week study, with a user engagement rate of 6.5 days per week and an average of 8.9 missions completed per day. According to the clinicians, a key success factor of the app lies in its ability to be personalised to the individual patient, and having a holistic approach to therapy management beyond medication intake by considering the psychological and lifestyle factors that strongly influence the condition. Overall, the study findings showed that digital solutions can significantly improve adherence and therapy outcomes for patients with AD through interventions to promote behavioural modifications toward higher disease awareness, treatment adherence and self-efficacy.4
HOW DIGITAL SOLUTIONS CAN DRIVE ADHERENCE FOR SELF-INJECTION THERAPIES
For patients prescribed an injectable drug for at-home treatment, device and injection training, management of injection-related stress and the establishment of an injection routine are key factors for successful treatment initiation and continuation. Most patients are left to execute their medication taking schedule on their own. Additionally, some patients may also experience anxiety around self-injection and express concerns around spillage, pain or fear of needles.5
“Management of injection-related stress and the establishment of an injection routine are key factors for successful treatment initiation and continuation.”
To address these challenges, digital therapy management applications for self-injection therapies should include an injection-specific experience, including features that purposefully engage with these challenges. By including important information about device characteristics, instructions for use, educational content and coaching about self-injections and selfmanagement, a digital injection module can provide great support to the user in their ability to self-inject and manage their treatment journey. The following sections describe in more detail selected use cases of the digital injection module being developed by Sidekick and Ypsomed.
Injection Training and Coaching
During the treatment initiation phase, patients require self-injection training to be confident in the use of their injection device to overcome any concerns regarding the safe delivery of the drug. However, in practice, many patients report a lack of injection training and onboarding to the device.6 Video-based injection training embedded into the therapy management application, in addition to a demonstration by a nurse, has shown to be effective and appreciated by patients.5 Combining this with a connected injection device that provides follow-up guidance can further enhance the patient experience.
Accordingly, educational materials in video format, interactive images, text or quizzes around how to prepare for the injection, the injection process itself and management of injection site reactions are key elements of a digital injection module with the aim of reducing use errors and early therapy drop-offs and improving adherence. To optimise the benefits to the patient and cover individual needs and questions, digital tools should be complemented with human coaching. In this way, the patient can get the best of both worlds. Many questions and challenges will be covered by the digital educational materials, allowing the human coaches to support many more patients than without a digital injection module.
“Combining connected injection devices with digital solutions is seen as an effective way to drive therapy outcomes.”
Reminders and Habit Building
Many patients prescribed an injectable drug suffer from comorbidities, which makes therapy management even more complex and challenging. Accordingly, a digital therapeutic should be capable of personalisation to the individual patient’s experience and cover several comorbidities within the same application. Easily configurable reminders and tips on how to set up an injection routine are helpful tools to manage the treatment schedule.
In addition, the integration with connected injection devices allows automatic tracking of injections and summarises them in a medication logbook within the app. First, this simplifies users’ lives as it takes away the cumbersome task of logging injections manually. Second, studies have shown that tracking medication intake has a significant effect on medication adherence.7 Showing progress, tracking flares and providing treatment goals powered by altruistic rewards can increase users’ motivation and engagement. Over time, establishing an injection routine can further simplify the injection journey by significantly reducing the cognitive effort required by the patient to plan and perform the injections.
Management of injection-related stress and anxiety
Another key area where a digital injection support module can provide significant value to the patient is the management of injection-related stress and anxiety. Despite the advantages in convenience and usability, at-home administration undeniably places a significant burden of responsibility on patients. Accordingly, there is a range of emotional aspects related to self-injection, such as concerns about incorrect technique, anxiety from needles and pain, lack of self-confidence and frustration with illness and treatment.8
A digital injection module can address these challenges by providing useful stress management and relaxation techniques before and after injections. Sidekick’s digital health platform is designed to address these factors through cognitive behavioural tasks that promote stress management and thought restructuring. In addition, patients are educated in dealing with negative feelings and stigma and are given the tools to cope with their condition. Last but not least, personal rituals before and/or after self-injection have been shown to be effective measures to reduce the cognitive load and injection-related anxiety.8

Figure 3: Ypsomed’s connected devices and therapy management solution with Sidekick.
SUMMARY AND CONCLUSION
Living with a chronic disease, such as AD, poses a huge burden on a patient’s life. Adherence to treatment, as well as adjusting habits, are of great importance. Using a digital application to support this and complement the medication-based treatment has proven to be effective, as Sidekick Health has shown in a recent study.
Self-medication for diseases like AD offers great advantages to patients and the healthcare system at large. However, there are also several challenges associated with it, from adherence issues to the lack of support patients receive. Together with Sidekick, Ypsomed aims to resolve these challenges by offering a digital module supporting selfinjection within Sidekick’s existing product.
Combining connected injection devices with digital solutions is seen as an effective way to drive therapy outcomes (Figure 3). Combining digital and device solutions is set to be a winning formula to deliver substantial value for the pharmaceutical industry, patients and the entire healthcare system.
REFERENCES
- Hadi HA et al, “The epidemiology and global burden of atopic dermatitis: a narrative review”. Life, 2021, Vol 11(9), p 936.
- Berke R, Singh A, Guralnick M, “Atopic dermatitis: an overview”. Am Fam Physician, 2012, Vol 86(1), pp 35–42.
- Frazier, Bhardwaj N, “Atopic dermatitis: diagnosis and treatment”. Am Fam Physician, 2020, Vol 101(10), pp 590–598.
- Gudmundsdóttir SL et al, “Clinical Efficacy of a Digital Intervention for Patients with Atopic Dermatitis: a Prospective Single-Center Study”. Dermatol Ther, 2022, Vol 12(11), pp 2601–2611.
- Homer Dawn, “Using video‐based training for button‐free auto‐injection of subcutaneous methotrexate: A pilot study”. Musculoskelet Care, 2019, Vol 17(3), pp 247–279.
- Miller E, “Applying Connectivity to Enhance the Training Standard of Care for Self-Injecting Drug Delivery Devices”. ONdrugDelivery, Issue 108 (June 2020), pp 43–46.
- Koledova E, Tornincasa V, van Dommelen P, “Analysis of real-world data on growth hormone therapy adherence using a connected injection device”. BMC Medic Inform Decis Mak, 2020, Vol 20(1), pp 1–7.
- Coyne M et al, “Impact of Routines and Rituals on Burden of Treatment, Patient Training, Cognitive Load, and Anxiety in Self-Injected Biologic Therapy”. Patient Prefer Adher, 2022, Vol 16, pp 2593–2607.


