Citation: Catino A, “Platform Training Solutions Add Value for Pharmaceutical Companies”. ONdrugDelivery, Issue 117 (Mar 2021), pp 72–74.
Alex Catino discusses the unmet need in healthcare for proper patient onboarding and training in the field of prefilled syringes and injection devices. Ms Catino uses Noble’s training device for Ypsomed’s YpsoMate® autoinjector as a case study for how bespoke training devices can be used to help improve the patient experience and adherence rates.
“Don’t practise until you get it right. Practise until you can’t get it wrong”, is a saying often associated with athletes and entertainers, but one that can also apply to the healthcare industry, especially to patients who use prefilled syringes and injection devices to self-administer their prescribed medications.
BREAKING DOWN BARRIERS TO PATIENT ADHERENCE
“One issue that often arises is the fear of needles, known as trypanophobia. The Diagnostic and Statistical Manual of Mental Disorders recognises it as a phobia that affect approximately 50 million Americans, making it a top-10 fear.”
With an increasing number of biologic medicines and drug delivery device options entering the market in recent years, pharmaceutical companies are making it possible – and more easily accessible – for patients to self-administer their drug therapies at home.
While self-injecting prescribed biologics at home is more convenient for both patients and their healthcare providers (HCPs) than having to do so in a hospital environment, it also comes with its own unique set of challenges. Overall, when patients are put in charge of administering their own medication, there is a tendency for patients’ adherence to their therapies to suffer. One issue that often arises is the fear of needles, known as trypanophobia. The Diagnostic and Statistical Manual of Mental Disorders recognises it as a phobia that affect approximately 50 million Americans, making it a top-10 fear.1 Anxiety when it comes to needles is also attributed to causing nearly half (45%) of patients who rely on self-injection therapies to either skip or cease their injections.2
Another phenomenon working against patient adherence to self-injection is the “forgetting curve”, which suggests that retention and recall worsen over time without practice and repetition. This theory postulates that 50% of the information patients receive from their HCP is forgotten within an hour. After that, patient memory declines rapidly by 80% in two days, with 90% of the information forgotten in a week.3
As biopharmaceutical companies develop therapies that permit longer intervals between injections – and therefore an improved patient experience, with patients injecting fewer times throughout the overall course of their therapy – the risk becomes greater that patients will forget critical steps for proper injection, and thus administer their therapies incorrectly, potentially resulting in a lack of treatment efficacy, and lose the confidence they need to self-inject.
Finally, telemedicine is poised to transform the healthcare landscape as a mainstream alternative to traditional in-person methods of care delivery. The use of this remote healthcare technology grew from less than 1% of primary care visits before the covid-19 pandemic to nearly 43.5% by April 2020.
Based on this current trajectory and rapid adoption rate, the continued, sustained growth of telemedicine is predicted for years to come.4 Of concern, however, is a report that found over 40% of people worry about their ability to obtain a proper diagnosis or treatment in a virtual setting.5 This apprehension is well placed, especially for patients with chronic conditions who must self-administer their medication at home. This is compounded by a study conducted by Noble that revealed that nearly half of patients who self-inject receive no training on how to do so properly.
TRAINING DEVICES DELIVER LASTING BENEFITS FOR PATIENTS AND HCPS

Figure 1: Noble’s YpsoMate® training device.
When it comes to HCPs prescribing self-injected medications to treat chronic illnesses such as ulcerative colitis or rheumatoid arthritis, training devices need to be part of the protocol. Evidence has shown that issues arise for patients who do not receive proper training:
- 84% make errors when using their autoinjector devices
- 74% discontinue their biologic medication regime at least once
- 45% skip or avoid their injections due to fear or anxiety.
A Noble-conducted survey of HCPs who work with patient groups most often prescribed self-injectable biologics found that, while HCPs value training for their patients, they are still not providing it. Why? The primary reason is that HCPs themselves are not being trained on the proper use of the drug delivery device. However, 71% of HCPs said they would be “very likely” to prescribe their patients a self-injected medication that came with a robust training solution.
Drug delivery training devices – including prefilled syringe and autoinjector training devices – provide the practice necessary for patients to overcome their anxieties about the self-injection process, and thus administer their medications confidently and consistently. Coupled with a robust onboarding programme, these training devices can help patients adhere to their therapies longer, resulting in improved health outcomes (Figure 1).
PARTNERING WITH BIOTECH COMPANIES TO DELIVER PLATFORM DEVICE TRAINING SOLUTIONS
Given that 49% of patients who are prescribed injection-based therapies do not receive training in an HCP’s office, and 90% of treatment information is forgotten within a week, it’s imperative that pharmaceutical companies take a holistic approach to ensuring that patients are familiar and confident with the use of their devices, understand their condition and treatment plan, and become and remain adherent to their therapy.
YpsoMate® Autoinjector Platform
“A Noble-conducted survey of HCPs who work with patient groups most often prescribed self-injectable biologics found that, while HCPs value training for their patients, they are still not providing it. Why?”
An example of this principle in practice is the fruit of Noble’s partnership with Ypsomed, a diabetes specialist and a developer and manufacturer of injection and infusion systems for self-medication. Noble’s injection training platform is based on Ypsomed’s YpsoMate® autoinjector – an automated, disposable injection device for 1 mL and large-volume 2.25 mL prefilled glass or polymer syringes, suitable for all patient groups – and designed to Ypsomed’s device specifications.
Noble’s YpsoMate® training platform replicates the real autoinjector device and incorporates proprietary features that are intended to give patients a realistic and repeatable simulated injection experience, including:
- Low reset forces
- A variable plunger speed system
- Device replication designed to demonstrate an actual drug delivery experience for patients.
There is also an option to incorporate a patented agitator tip designed for those 45% of patients who have a fear of needles. This feature slightly pricks – but does not at all puncture – the skin at the start of the injection to create the sensation at the injection site. The training device also allows for varying needle forces and ranges, depending on what the pharma company needs to best replicate its drug delivery device injection experience (Figure 2).
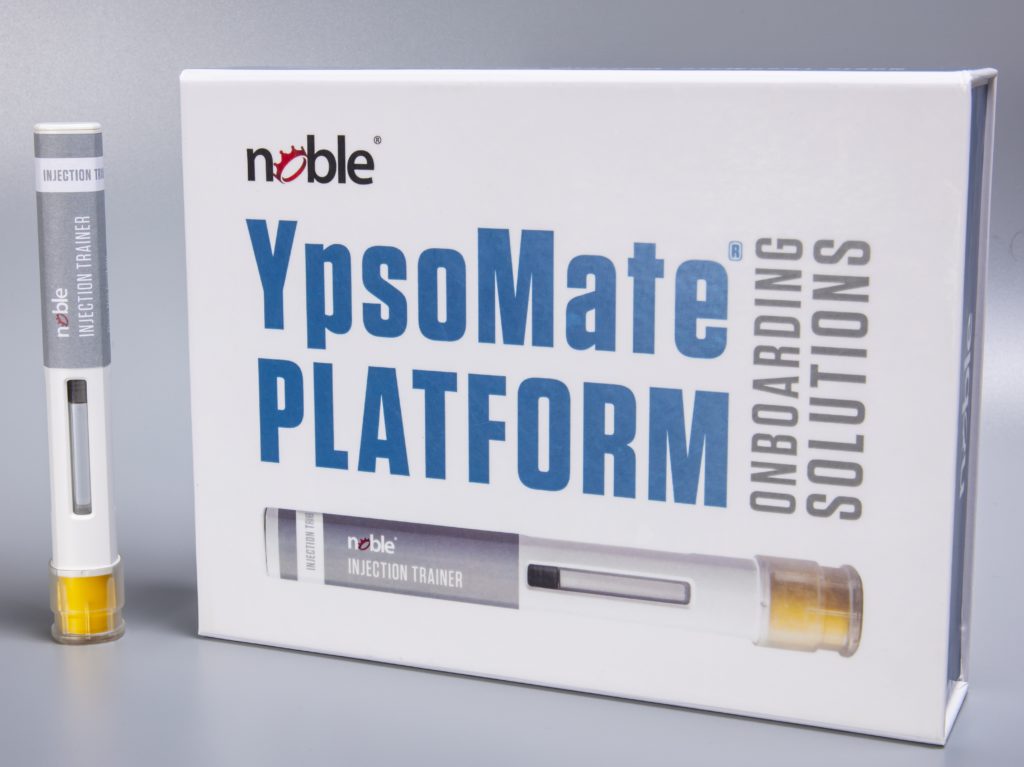
Figure 2: Noble’s YpsoMate® training solutions, which include training devices and instructions for use in high-quality packaging.
In addition to the patient benefits and training device design technologies, Noble’s YpsoMate® platform programmes also provide several benefits for individual brands, including:
- High speed-to-market
- Lower cost of entry
- The ability of brands to customise training devices to meet their unique specifications.
CONCLUSION
When it comes to using prefilled syringes and injection devices to self-administer prescribed medications, half of all patients are non-adherent due to gaps in their treatment experiences. The cost of this non-adherence and non-optimised therapy is steep – estimated at US$528 billion (£385 billion) annually – and everyone pays the price, from biopharmaceutical brands and payers to HCPs and their patients.6 It has been shown that injection device training can result in a decrease of up to 85% in patients who abandon their treatment regimen, making training devices critically important for the millions of patients across the globe who live with chronic illnesses.7
Finally, Noble also offers clients a full lifecycle of supporting solutions – from development to commercialisation – including market research, logistics management, training and product launch strategy services to further support pharma brands.
In much the same way that telemedicine is transforming healthcare delivery, training platforms and services are poised to change the future of adherence and onboarding through research-driven insights, innovative technologies and patient-focused solutions, helping patients practise until they can’t get it wrong.
REFERENCES
- “Fear of Needles: The Fatal Phobia”. PharmaJet blog, Nov 2013.
- Guilliouma W, “Sensor Advancements in Drug Delivery Improve Compliance”. ONdrugDelivery Magazine, Issue 107 (May 2020), pp 25–28.
- Kohn A, “Brain Science: The Forgetting Curve–the Dirty Secret of Corporate Training”. Learning Solutions, Mar 2014.
- “Predicting the Future Role of Telemedicine”. Modern Healthcare, Oct 2020.
- “Survey Report: Americans’ Perceptions of 5G Technology”. Skyes, 2020.
- Watanabe JH, McInnis T, Hirsch JD, “Cost of Prescription Drug–Related Morbidity and Mortality”. Ann Pharmacother, 2018, Vol 52(9), pp 829–837.
- Mease P et al, “Impact of a Patient Support Program on Abandonment of Adalimumab Treatment Initiation in Patients with Rheumatoid Arthritis, Ankylosing Spondylitis, and Psoriatic Arthritis”. Arthritis Rheumatol, 2016, 68 (suppl 10).



