To Issue 156
Citation: Rahman O, Desai M, Candiotti K, “Beyond the Point: Navigating the Impact of Needles on Pain, Anxiety and the Patient Experience”. ONdrugDelivery, Issue 156 (Jan 2024), pp 40–43.
Omar Rahman, Mehul Desai and Keith Candiotti discuss the role that needle size plays in the pain and anxiety patients experience during injections and how smaller, hidden needles (30G), such as those employed by Enable Injections‘ enFuse large-volume injector, may minimise patient discomfort and maximise subcutaneous injection efficiency.
Over the last decade, the subcutaneous (SC) administration of therapeutics has experienced significant growth, emerging as a widely accepted option for drug delivery. The shift from intravenous (IV) infusions to SC injections has not only reduced the drug administration burden on the healthcare system, but is also generally preferred by patients and healthcare practitioners (HCPs).1–4 This positive impact has led to intensified research aimed at understanding the key elements of the SC administration process, such as the impact of needle size, needle phobia and environment, on the overall patient experience.
The choice of needle size can significantly influence the patient experience, particularly when larger diameters are employed. Larger needle diameters have been associated with heightened levels of pain and anxiety in patients, casting a shadow across the overall quality of care. The discomfort induced by needles not only amplifies the immediate physical sensations, but also contributes to long-lasting psychological repercussions, potentially leading to or exacerbating needle phobia.
“Aversion to needles not only poses challenges for HCPs but also jeopardises the overall wellbeing of patients, as essential treatment may be delayed or avoided altogether.”
Needle phobia, characterised by an intense fear and anxiety of needles, is a prevalent concern that further complicates the patient experience. The widespread prevalence became evident in a recent global survey conducted among a general adult population (N = 2,098), where 63% of participants reported experiencing needle phobia.5 Individuals afflicted by needle phobia may exhibit heightened anxiety, increased heart rate and even avoidance behaviours. Aversion to needles not only poses challenges for HCPs but also jeopardises the overall wellbeing of patients, as essential treatment may be delayed or avoided altogether.
When delving into the impact of larger needle diameters, needle phobia and the environment on the patient experience, it becomes imperative to explore strategies and innovations that mitigate these adverse effects. By understanding the psychological and physiological dimensions of needle-related distress, HCPs and injection-system manufacturers can begin to tailor interventions to minimise pain, alleviate anxiety and enhance the overall SC administration experience for patients.
“63% of insertions with 23G needles caused pain, compared with 53% with 27G needles and 31% with 32G – the thinnest needle.”
NEEDLE SIZE AND PAIN
The impact of needle size on pain during SC administration is a critical consideration, as highlighted in research by Arendt-Nielsen et al and Præstmark et al.6,7 These studies emphasise the significant correlation between the outer needle diameter and the frequency of pain, shedding light on the direct relationship between needle characteristics and the patient experience.
The study conducted by Arendt-Nielsen et al specifically looked at the association between the outer needle diameter and the frequency of insertion pain during SC administration among healthy volunteers.6 The results revealed a positive and statistically significant correlation, underscoring the influence of needle size on pain perception. Notably, the study demonstrated that larger needle diameters were associated with a higher frequency of insertion pain. For instance, 63% of insertions with 23G needles caused pain, compared with 53% with 27G needles and 31% with 32G – the thinnest needle. This clear trend emphasises the importance of considering needle diameter as a crucial factor in predicting and managing pain during SC administration.
Examining the data in detail reveals a more significant reduction in pain perception when transitioning from a 27G to a 32G needle size (22%) compared with the difference observed from a 23G to a 27G needle (10%). This finding prompts the intriguing consideration of a potential threshold effect, indicating that pain becomes notably more apparent at the 27G mark. Another study, conducted by Præstmark et al, lends support to the existence of another threshold effect, suggesting that the 30G needle size represents the point with the least impact on pain.7 Beyond this threshold, going to needle sizes smaller than 30G does not seem to yield any noticeable impact on pain perception. This conclusion is based on observations where there was no significant difference in pain scores or the increase in skin blood perfusion (SBP) between a 32G and 30G needle.
To reinforce this argument, Yomtoob et al conducted a study specifically addressing periocular injections, a notably sensitive area around the eyes.8 The findings revealed no noticeable distinction in pain scores between the use of a 32G needle and a 30G needle. The lack of distinction in pain perception when going beyond 30G could be attributed to the subjects’ limited ability to differentiate between needles when they fall below a certain size. This finding strongly suggests that the 30G needle size represents a point at which the impact on pain is notably minimal, potentially serving as a threshold for optimising patient comfort during SC administrations.
Præstmark et al also explored the relationship between needle diameter and both penetration force (PF) and SBP.7 The study revealed positive correlations between needle diameter and both PF and SBP, indicating that larger needles require more force for penetration and are associated with higher levels of local tissue trauma. Additionally, the findings indicated a positive trend in relation to pain, further highlighting the impact of needle diameter on pain perception during SC administrations.
“Recognising and addressing visible aspects of the administration process is crucial for HCPs to implement strategies that enhance the overall patient experience and alleviate anxiety and pain.”
The research findings collectively suggest that thinner needles are associated with less pain during SC injections. Reduced needle thickness not only results in diminished pain but also requires a lower PF. This aligns with the broader understanding that minimising tissue trauma and nerve stimulation via less force contributes to a more favourable patient experience. Both studies’ positive correlations between outer needle diameter and insertion pain frequency emphasise the need for thoughtful consideration of needle characteristics in injection-system development and clinical practice.
NEEDLE PHOBIA
The impact of needle phobia associated with drug administration via needle is a multifaceted challenge with far-reaching implications for patient wellbeing and healthcare delivery. The study by Albrooks et al sheds light on the prevalent reasons behind needle fear, highlighting the intricate relationship between general anxiety, pain and the complex aetiology of needle phobia.5 Among the participants experiencing needle phobia, general anxiety (96.1%) and pain (95.5%) emerged as the most common reasons for their fear of needles. This emphasises the pervasive nature of anxiety in the context of needle-related procedures and underscores the need to better understand the factors contributing to anxiety and, ultimately, needle phobia.
Albrooks et al examined various factors that positively correlate with needle phobia.5 Notably, “non-needle-related medical fears” was the highest positively correlated independent variable with needle phobia, which suggests a broader context of anxieties associated with the wider administration process and healthcare system. Coupled with the common selection of “distractions” and “relaxation techniques” as top non-device-related strategies to cope with needle phobia, this aligns with the overarching argument that visibility of the administration process plays a pivotal role in shaping a patient’s level of anxiety, which has direct implications for comfort and compliance.
Another crucial aspect highlighted in the study was the identification of potential device-related solutions to alleviate fear, which included “non-invasive alternatives” (94.1%) and the use of “smaller needles” (91.1%) as the most commonly suggested strategies. Another study by Jaber et al adds further weight to this argument, demonstrating that injections using needles with thermoplastic elastomer shield material were consistently perceived as less painful than those with rubber needle shields, irrespective of variations in needle diameter.9 This reinforces the link between the visibility of different administration aspects, the perceived level of anxiety and, ultimately, pain.
Collectively, these findings validate the pivotal role of a patient’s level of anxiety and pain triggered by the visibility of the administration experience and interaction with the wider healthcare system. Recognising and addressing visible aspects of the administration process is crucial for HCPs to implement strategies that enhance the overall patient experience and alleviate anxiety and pain.
SAFETY
The relationship between smaller needle sizes and fewer safety events is underscored by compelling data, as indicated in the study by Jaber et al.9 Specifically, when patients self-administered interferon beta-1a using a 29G needle compared with a 27G, not only was there a notable reduction in reported pain, but patients also experienced fewer safety events. The survey revealed a significant decrease in bruising, burning, stinging and injection-site reactions associated with the use of the smaller 29G needle.
These data support the notion that the adoption of smaller needle sizes in SC drug delivery addresses patient comfort by minimising pain, but also contributes to a more favourable safety profile. These results are consistent with prior evidence by Præstmark et al, demonstrating that smaller needles lead to reduced tissue trauma and provoke gentler physiological responses, which are crucial elements in the overall development of injection-site reactions.7 Therefore, incorporating smaller needles in SC drug delivery has the potential to enhance patient comfort and concurrently promote safety.
“These data support the notion that the adoption of smaller needle sizes in SC drug delivery addresses patient comfort by minimising pain, but also contributes to a more favourable safety profile.”
ENFUSE TECHNOLOGY
Enable Injections’ novel enFuse® drug delivery system delivers high-volume therapeutics through SC administration, offering a more flexible alternative to IV administration and other currently available SC options, such as infusion pumps. Among its numerous advantages, the enFuse system features a remarkably small, 30- to 31-gauge ultra-thin-walled and hidden needle (30G for discussion in this article), directly addressing patient needs regarding the pain and anxiety associated with the administration process (Figure 1).
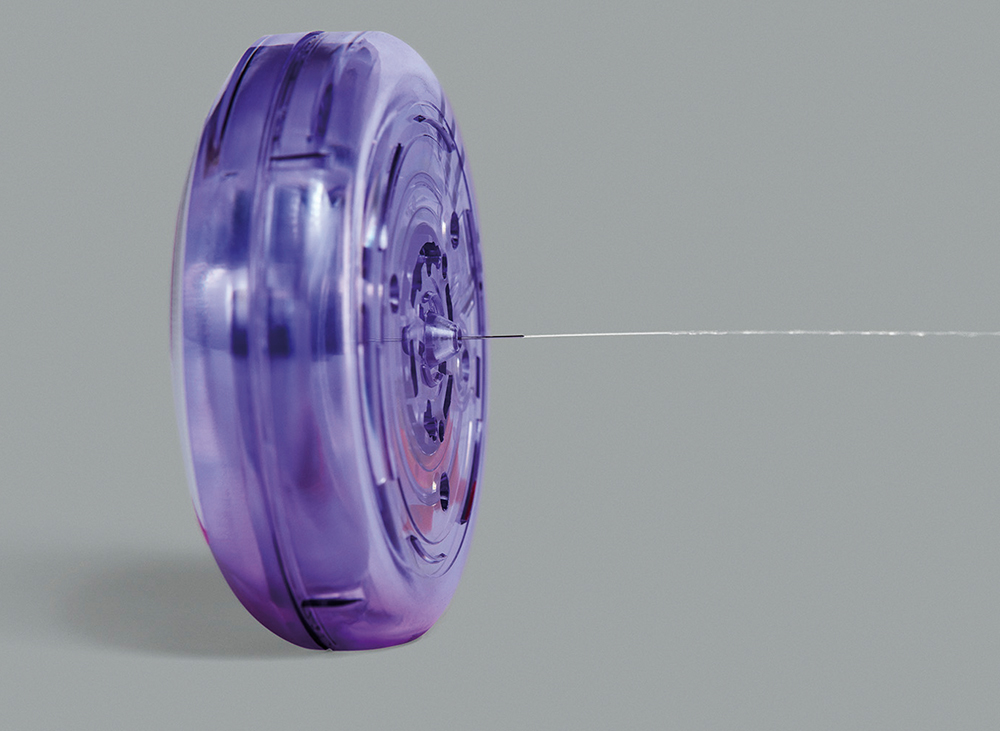
Figure 1: Among its numerous advantages, the enFuse system features a remarkably small needle (30G) that is hidden from the user throughout the entire administration process.
“In the pursuit of expediting delivery times, the reliance on larger needles in large-volume SC delivery has inadvertently compromised the overall patient experience.”
A cross-over study comparing enFuse with the Crono Pump (Canè Medical Technology) among patients with primary immunodeficiency vividly illustrates the real-world impact of using smaller, hidden needles. For SC administration of immunoglobulin G with the enFuse (30G needle), the incidence of most injection site reactions was notably lower than with the Crono Pump (26G needle). Specifically, the percentage of any injection-site reaction for all infusions was 3.4% for the enFuse and 6.7% for the Crono Pump. A parallel safety trend was observed in a separate study involving the enFuse, demonstrating excellent local tolerability with only seven injection site reactions out of 404 administrations (1.7%) – all of which were Grade 1.10
In terms of pain perception, the cross-over study involved patients listing their reasons for preferring the enFuse over the Crono Pump. Nearly 50% of patients chose “causes less pain at the injection site” as one of their top reasons – a direct testament to the positive impact of enFuse’s smaller and hidden needle feature on patient comfort and pain.10 The advantages of the hidden needle feature extend beyond patients to include payers, who recognise a distinct link between the hidden needle and potential improvements in treatment adherence. Notably, in a preference study for the enFuse, payers ranked the hidden needle among the primary advantages of the wearable system.4 The enFuse technology also stands out with its unique constant-pressure design, employing elastomeric technology rather than a constant-flow design via an electromechanical pump. This distinctive approach enables the enFuse system to dynamically adjust to the back pressure at the injection site, potentially reducing pain even further in conjunction with its small, hidden needle.
In the elastomeric constant-pressure design, the needle serves as the flow restrictor, allowing for the adjustment of various flow rates by modifying needle features, such as diameter and length. The distinctive design of the enFuse flow restrictor has enabled minimal alteration to the needle outer diameter, maintaining it at or around a conventional 30G, while adjusting the inner diameter to meet the desired delivery time. This adaptability emphasises the versatility and accuracy of the enFuse technology, giving partners the tools to tailor drug delivery and address the unique requirements of specific patient groups.
In the pursuit of expediting delivery times, the reliance on larger needles in large-volume SC delivery has inadvertently compromised the overall patient experience. The emphasis on faster administration, without due consideration for the associated discomfort, underscores the need for a paradigm shift towards prioritising patient comfort in SC administration. Moving forward, a re-evaluation of needle size choices is imperative to align SC drug delivery with a more patient-centric approach, ensuring that advancements in delivery speed do not come at the expense of the patient’s wellbeing. By fostering a balance between efficiency and patient experience, the enFuse can pave the way for more comfortable and effective healthcare practices in large-volume SC drug delivery.
REFERENCES
- Pivot X et al, “Patients’ preferences for subcutaneous trastuzumab versus conventional intravenous infusion for the adjuvant treatment of HER2-positive early breast cancer: final analysis of 488 patients in the international, randomized, two-cohort PrefHer study”. Ann Oncol, 2014, Vol 25(10) pp 1979–1987.
- De Cock E et al, “Time Savings with Rituximab Subcutaneous Injection versus Rituximab Intravenous Infusion: A Time and Motion Study in Eight Countries”. PLoS One, 2016, Vol 11(6), Article e0157957.
- Desai M et al, “Monoclonal antibody and protein therapeutic formulations for subcutaneous delivery: high-concentration, low-volume vs. low-concentration, high-volume”. Mabs, 2023, Vol 15(1), Article 2285277.
- Desai M, “Exploring US Payer Perspectives on a Large-Volume Subcutaneous On-Body Delivery System: A Double-Blinded Preference Study”. Poster, PDA Universe of Pre-Filled Syringes and Injection Devices Conference, Gothenburg, Sweden, Oct 2023.
- Alsbrooks K, Hoerauf K, “Prevalence, causes, impacts, and management of needle phobia: An international survey of a general adult population”. PLoS One, 2022, Vol 17(11), Article e0276814.
- Arendt-Nielsen L, Egekvist H, Bjerring P, “Pain following controlled cutaneous insertion of needles with different diameters”. Somatosens Mot Res, 2006, Vol 23(1–2), pp 37–43.
- Præstmark KA et al, “Pen needle design influences ease of insertion, pain, and skin trauma in subjects with type 2 diabetes”. BMJ Open Diabetes Res Care, 2016, Vol 4(1), Article e000266.
- Yomtoob DE et al, “Comparison of pain scores with 30-gauge and 32-gauge needles for periocular botulinum toxin type a injections”. Ophthalmic Plast Reconstr Surg, 2009, Vol 25(5), pp 376–377.
- Jaber A et al, “A novel needle for subcutaneous injection of interferon beta-1a: effect on pain in volunteers and satisfaction in patients with multiple sclerosis”. BMC Neurol, 2008, Vol 8, Article 38.
- Wasserman RL et al, “Systemic IgG exposure and safety in patients with primary immunodeficiency: a randomized crossover study comparing a novel investigational wearable infusor versus the Crono pump Systemic IgG exposure and safety in patients with primary immunodeficiency: a randomized crossover study comparing a novel investigational wearable infusor versus the Crono pump”. Immunotherapy, 2022, Vol 14(16), pp 1315–1328.

