Citation: Miller E, “Training Devices Increase Patient Engagement and Adherence – Creating Better Outcomes”. ONdrugDelivery Magazine, Issue 97 (May 2019), pp 47-50.
Erin Miller outlines a study looking at how patients interact with training resources during the first 14 days of a new treatment – and how training devices can help increase confidence, adherence and, ultimately, overall outcomes for the millions of patients who manage their diseases through self-injection.
Across the US, half of all adults live with a chronic disease – and many of them are prescribed a self-injectable therapy to help manage their condition. As the patient population and demand for self-injection treatments continue to grow, so will the number of patients being introduced to self-injection drug delivery devices. This growing trend increases the importance of effective training and the onboarding process (the first 30-90 days of treatment) as more patients find themselves self-managing their treatments away from clinics.
“Lack of training, among other
factors, has led to 84% of patients
incorrectly administering their
medication with an autoinjector.”
Unfortunately, even with this growth in prescribed self-injectables, 49% of these patients are not trained in a healthcare provider’s (HCP’s) office. What’s more, 43% of HCPs have not received training devices themselves – limiting their ability to train patients from the very beginning.1 This lack of training, among other factors, has led to 84% of patients incorrectly administering their medication with an autoinjector.2 Additionally, it has been found that patient nonadherence – whether from a lack of training in an HCP’s office, the absence of training devices in the home or patients not reading the instructions for use (IFU) – costs the pharmaceutical industry approximately US$637 billion (£492 billion).3
THE FORGETTING CURVE
he forgetting curve – which asserts that, without practice and repetition, memory retention and recall degrade over time – has an important impact on patient adherence. This decline in retention and recall can result in an increase in device usage errors, such as injecting at the wrong angle or removing the device prematurely from the injection site, thereby increasing overall nonadherence to treatment (Figure 1). The forgetting curve suggests that 50% of information is forgotten within one hour – and 90% within one week – after training with an HCP.4 Patients can work to reverse these statistics by having training devices on hand at home to practise with throughout the course of their therapy.
“The forgetting curve suggests that 50% of information is forgotten within one hour – and 90% within one week – after training with an HCP.”
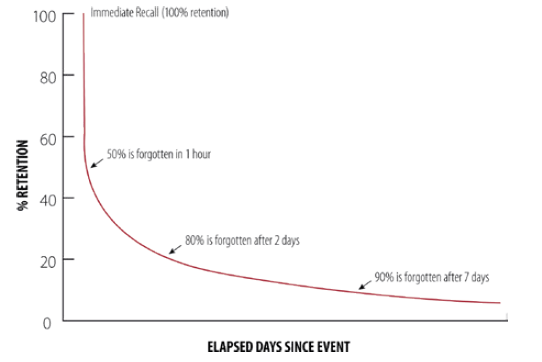
Figure 1: The forgetting curve asserts that, without practice and repetition, memory retention and recall degrade over time.
Noble conducted a study that set out to confirm and then shed light on these real patient issues and show how training devices can help increase confidence, adherence and, ultimately, overall patient outcomes for the millions of patients who manage their diseases through self-injection.
STUDY METHODOLOGY
Over the years, Noble has conducted multiple cross-sectional studies to understand patient onboarding needs and how training could be used to increase confidence and decrease anxiety. Using these research outputs as a foundation, Noble launched a first-of-its-kind longitudinal training device study to learn more about patient recall, retention, adherence, engagement and more. The study, which was sponsored by Noble and conducted by Insight Product Development, explored three conditions as they relate to the performance, engagement and preferences of injection-naïve people experiencing a self-administered injection for the first time. Researchers sought to understand how patients interact with training resources during the first 14 days of treatment.
To do so, the study employed a 14-day decay period, which was used to mimic a common fortnightly injection frequency. Specific objectives of the study included:
- Assessing the effects of different training materials on self-injection performance
- Understanding how patients engage and interact with training materials
- Evaluating the effects of different training materials in relation to patient confidence, anxiety, preparedness, preference and potential compliance.
To create the most realistic onboarding experience for participants, the study employed a deception paradigm to ensure participants would practise at home throughout the study in the same way they would if they were truly onboarding to a new self-injection therapy. Participants were told they would be injecting themselves using a real autoinjector during the second session. Because of this paradigm, the study protocol was reviewed and approved by a third-party institutional review board.

Figure 2: A participant injects with a training device on an injection pad.
The study comprised 27 healthy adults – with no prior knowledge of self-injections or formal training as an HCP – randomly assigned to one of three cohorts. Each cohort was assigned different training stimuli for use during the decay period.
THE STUDY
To begin the study, participants across the three cohorts attended an introductory session where they received self-injection training, just as they would in a doctor’s office if they were prescribed a self-injection course of therapy.
During this first session, researchers replicated an optimal introductory in-office learning experience between an HCP and a patient. This session focused on introducing participants to the drug delivery device and then training them on how to use it with a device that did not include medication or a needle (Figure 2). Afterwards, participants could practise on themselves with a training device, with researchers present. Participants were also given feedback and recommendations for improvement, as would occur during training with an HCP. After the 45-minute training session, they were sent home.
To understand the effects of having access to a training device in-office only, cohort A – the control group – was sent home with only an IFU. This cohort was not intended to represent the minimum amount of training a patient may receive but to set a baseline for evaluating the effects of having additional support, such as training materials, at home. Cohort B was sent home with both an
IFU and a training device that mimicked the actual device they would self-inject with later in the study. Cohort C was given both the IFU and the training device, as well as an interactive training video to use at home (Figure 3).
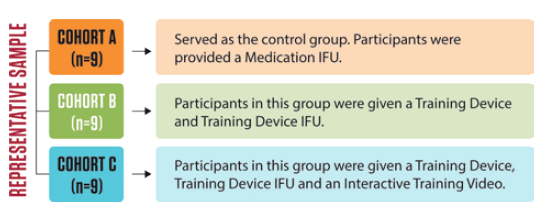
Figure 3: Twenty-seven participants were randomly assigned to one of three cohorts with various training materials.
Participants were instructed to practise at home as little or as often as they preferred and were told to keep track of how many times they used their materials.
Participants then did not hear from researchers for 14 days, allowing them to practise with the various materials as frequently or infrequently as they preferred. The purpose of this was to uncover the correlation between successful and unsuccessful self-injections and subjects’ access to training materials.
FINDINGS HIGHLIGHT NEED FOR TRAINING DEVICES
Following a 14-day decay period, researchers conducted a second session to evaluate participants’ ability to recall the correct self-injection technique properly with an actual device.
During this follow-up session, participants’ performance was evaluated based on their ability to self-inject successfully using an injection pad on their preferred site. Participants were asked to complete this evaluation under the observation of a human factors engineer. Critical steps evaluated were:
- Removing the cap
- Placing the autoinjector at a 90° angle
- Actuating the device by depressing the needle shield, and pushing and releasing the injection button
- Holding the autoinjector in place on the skin for the full injection duration.
TRAINING DEVICES HELP WITH SUCCESSFUL INJECTIONS
Overall, performance in self-administering the injection differed starkly between the three training groups. Those with training devices performed better – successfully completing all critical steps during their simulated injections.
The research found that 100% of cohorts B and C completed all critical steps for a successful self-injection, while only 44% did so from cohort A.
PATIENTS MORE ENGAGED WITH THEIR TREATMENT
“Engagement in general increased for participants who
had training devices to practise with at home.”
It was also found that engagement in general increased for participants who had training devices to practise with at home.
Participants in cohorts B and C prepared for their injection more often at home than those in cohort A, who only had an IFU. Cohorts B and C both saw 100% of participants practise at least three times – and, in the case of cohort C, 83% practised 5–9 times. This is in contrast with cohort B, where only 33% practised 5–9 times (Figure 4).
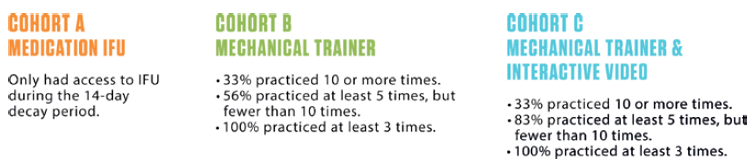
Figure 4: Research found participants with additional training resources were more engaged during the decay period.
RESEARCH SHOWS VALUE OF TRAINING DEVICES
The findings suggest that trainers and other support materials could be extremely valuable to patients who self-inject, as successful injection nearly doubles with training materials that go beyond the standard IFU. The vast majority of participants – 92% – reported that they would prefer to bring home a training device to practise with prior to conducting a self-injection (Figure 5).
“The findings from this study suggest that the implementation of training devices and their use in a home environment
helps the user perform successful self-injections.”
A participant from cohort A told researchers: “I would [have liked] the training device. If I had it, I would have remembered [important steps like] taking the cap off.” Similarly, a participant from cohort B told researchers: “The trainer device was helpful [because] you can actually practise and get to be hands-on.” Another participant from cohort B stated: “Taking the trainer home was so helpful. I was much more comfortable having it.”
SIGNIFICANT FINDINGS
Participants who did not have a training device at home had to rely on the experience of using the training device in the first session and on rote memory from reading the instructions – resulting in more critical errors relative to the other cohorts. With the training devices to take home, participants from cohorts B and C were able to practise and, as a result, build motor memory and improve performance. These participants were more confident about how to manipulate the device and the order in which they needed to perform tasks.

Figure 5: The vast majority of participants stated how important a training device would be to have in the home for practice.
Overall, giving a patient a training device that is close in design and function to the commercial device to practise with at home facilitates the development of a mental framework and motor memory conducive to a successful self-injection. It is also widely understood that learning the proper self-injection technique involves multiple practise sessions to get acquainted with the various steps involved, beyond that of practising with an HCP during an in-office visit. Having a training device to help with this memory reinforcement is crucial. This, in turn, proposes a critically important conclusion: when anxiety over self-injection is diminished, and patients have mastered the self-injection technique, they may have a higher likelihood of adhering to their treatment, thus obtaining the maximum benefit from it. In addition to having training devices for practice, research has also found that patients who are more involved in their healthcare experience achieve better outcomes and incur lower costs. These training devices help patients become – and stay – more engaged and involved, thus promoting adherence.
CALLS FOR IMPROVEMENT
To ensure successful self-administration techniques, patients and their HCPs should develop a strategy to improve therapeutic outcomes. An informed patient is essential for developing a framework focused on treating his/her illness and preventing behaviours detrimental to treatment. HCPs must also be informed of the existence of – and the need for – training devices and other materials. Overall, the findings from this study suggest that the implementation of training devices and their use in a home environment helps the user perform successful self-injections. This highlights the benefit of providing patients with training resources during the onboarding phase and beyond.
REFERENCES
- Lang VA, Nalan D, “Combination Product Patient Training: How Are Patients Trained and Who Conducts the Training?”. Proc 2018 Design of Medical Devices Conference (Am Soc Mechanical Engineers), April 9-12, 2018, Minneapolis, MN, US, DMD2018-6956.
- Potera C, “Misuse of Autoinjectors and Inhalers”. Am J Nursing, Vol 115(3), p17.
- “Pharmaceutical Companies Lose $637 Billion in Revenue Annually Due to Medication Nonadherence”. Press Release, HealthPrize Technologies, November 2016.
- Kohn A, “Brain Science: The Forgetting Curve –the Dirty Secret of Corporate Training”. Learning Solutions, March 13, 2014.

