Citation: Shain A, “Putting Their Health in Their Hands: Enhancing Respiratory Patient Outcomes Through Digital Therapeutics”. ONdrugDelivery, Issue 121 (Jun 2021), pp 32–36.
Adam Shain discusses the role digital therapeutics play in respiratory patient outcomes and looks at the potential for expansion into other therapy areas.
“Recent advances in drug and device development have enabled increasing numbers of patients to manage their health by controlling symptoms and responding to acute situations, thereby reducing the level of intervention required by HCPs in the process, and avoiding acute exacerbations and visits to A&E.”
For patients suffering from chronic respiratory diseases, the opportunity for greater control over their condition not only benefits their physical health but can also significantly enhance their overall quality of life.
Recent advances in drug and device development have enabled increasing numbers of patients to manage their health by controlling symptoms and responding to acute situations, thereby reducing the level of intervention required by healthcare professionals (HCPs) in the process, and avoiding acute exacerbations and visits to A&E.
As such, self-management is welcomed by most patients. Analysis of published reviews and syntheses of qualitative research related to 14 long-term conditions, including asthma and COPD, concluded that patients have a clear appetite for a better understanding about their illnesses, and desire stronger, more collaborative relationships with their HCPs.
While the patient is arguably the greatest benefactor in the self-care model, they can also be the greatest flaw. Due to the critical part they play in the process, patients can be a major barrier to success in therapy management if their behaviour does not correlate with the actions prescribed by HCPs.1
MANAGING PATIENT BEHAVIOUR
“Cohero Health®, an Aptar Pharma company, was founded in 2013 with a vision of transforming the traditional approach to respiratory disease management through smart mobile technologies. This vision resulted in the development of BreatheSmart®
a comprehensive digital therapeutics platform that enables patients and HCPs to better screen, track and manage asthma and COPD at a personalised level.”
Poor levels of adherence can be attributed to several factors, from poor engagement to low levels of motivation and lack of informational awareness. Confidence can also be an issue; patients suffering from long-term conditions have been found to be less self-assured in managing their health compared with the population at large. Furthermore, this confidence issue is most prevalent in older age groups, which represent the vast majority of people living with chronic conditions.2
For HCPs, there is currently very little that can be done to monitor and address these gaps in patients’ self-management regimes. Medical appointments provide important points of interaction, but they can be infrequent and relatively transient. These appointments therefore provide only limited opportunities to identify poor adherence, address the root causes and create individualised plans for behavioural change in the patient. The net result of this lack of touchpoints is evidenced through high levels of medicine wastage and missed opportunities for patients to optimise their self-management and improve their healthcare on an ongoing basis.
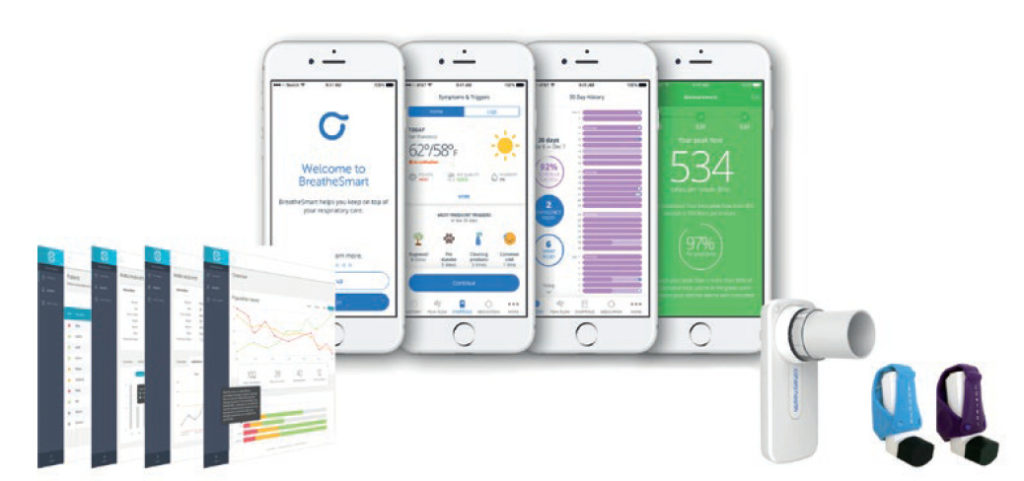
Figure 1. BreatheSmart® Connect digital health platform – a care co-ordination and HIPAA-compliant SaaS cloud service that captures and securely stores data from Cohero Health’s devices and BreatheSmart® software for remote monitoring and patient communications to help manage patient therapy.
In recent years, we have witnessed the introduction of several digital healthcare solutions designed to address some of these challenges. Cohero Health®, an Aptar Pharma company, was founded in 2013 with a vision of transforming the traditional approach to respiratory disease management through smart mobile technologies. This vision resulted in the development of BreatheSmart®, a comprehensive digital therapeutics platform that enables patients and HCPs to better screen, track and manage asthma and COPD at a personalised level (Figure 1).

Figure 2. BreatheSmart® app – designed for patient habit creation and behaviour change, driving appropriate medication use.
The BreatheSmart® app is designed for patient habit creation and behaviour change, driving appropriate medication use. The app provides real-time tracking of medication adherence and lung function, along with reminders, educational materials and symptom/trigger recording (Figure 2).

Figure 3. mSpirometer™ and cSpirometer™ lung function diagnostic sensors – enables comprehensive pulmonary lung function testing in a handheld wireless device.
PATIENT-CENTRIC DESIGN
The system incorporates all the hardware and software required to form an interactive digital environment between the patient and their HCP. This includes mSpirometer™, which details up to six different measurements, including FEV1, FVC and peak-flow volumes (Figure 3). The Bluetooth-enabled HeroTracker® is fitted to both control and rescue inhalers to record time and date of dose (Figure 4).
The main patient interface is a mobile app, available in iOS and Android versions, for real-time tracking of medication adherence and lung function, as well as the recording of symptoms and triggers, and the delivery of dosing reminders and educational materials. Due to the app’s pivotal role in trying to secure patient engagement and facilitate ongoing use of the system, great care was taken in the development of the interface to ensure it provided an intuitive experience for patients.
This was achieved by incorporating behavioural modelling alongside user interface and user experience design methodologies. Colour, for example, is used to provide a visual representation of peak-flow data, with the universally recognised RAG (red, amber or green) colour coding used in screen backgrounds to provide a clear indication of lung performance.
Ultimately, modelling such as this creates a platform that is accessible and helpful, as well as rewarding and enjoyable for patients.
Design was just one aspect of an extensive development and test process for BreatheSmart®, which also incorporated clinical input from pulmonologists, care guidance from regulatory bodies and feedback from extensive user and focus groups. Looking ahead, Aptar Pharma is committed to the continued development of the platform with a view to further exploiting the benefits for patients and HCPs.

Figure 4. HeroTracker® sensors – Bluetooth-enabled medication smart inhaler sensors designed for both control and rescue medications. They attach to respiratory medications to automatically record time and date of doses taken.
“Good communication is a crucial element on the journey to improving patient outcomes through digital healthcare services. BreatheSmart® supports effective communication by showing targeted educational information in text and video form.”
DRIVEN BY DATA
When in use, all patient data captured on the BreatheSmart® platform is stored on a secure cloud-based server designed to be HIPAA- and GDPR-compliant, accessible to patients and clinicians via the BreatheSmart® Connect interface. This provides a dashboard view of a patient’s medical information. The BreatheSmart® platform supports API-based integration with electronic health records to support a contextual view of patient information.
Because data is recorded in real time at the point of use, the platform can paint an accurate in-depth picture of an individual patient’s engagement with their medicine regime. This provides invaluable information for the HCP to understand and optimise therapy management.
While a great deal of the developments in digital healthcare to date have been aspirational and theoretical in nature, a commercial-stage product, such as BreatheSmart®, has been validated through actual use, in pharmaceutical research applications and clinical trials.
Analysis of real-world user data shows how BreatheSmart® has been overwhelmingly welcomed by patients, with a pleasing 92% user-satisfaction rate.3 Crucially, it has also been shown to improve adherence to medicine regimes by a factor of 3:1 and a user-retention rate of 72% after a year of use. This data demonstrates the platform’s ability to deliver long-term engagement as well as support a 95% reduction in the use of rescue medication, and a 50% reduction in A&E visits among users.
CONTROLLING LONG-TERM RISK
With higher levels of adherence comes better levels of self-care, leading to improved overall health and quality of life. From the perspective of a medical professional, better adherence also equates to greater control over a patient’s long-term risk.
As the severity of COPD increases over time, patient suffering increases exponentially as a direct result of their condition. They are also more likely to need to manage a range of associated health issues and complications. Examples include loss of mobility and weight gain, which almost inevitably lead to poor mental health, including anxiety and depression. Ever more complex medical needs correlate with an increase in the overall cost of care. This is just one more reason why connected digital platforms, such as BreatheSmart®, are critical to delivering cost savings alongside the proven health benefits.
Good communication is a crucial element on the journey to improving patient outcomes through digital healthcare services. BreatheSmart® supports effective communication by showing targeted educational information in text and video form. The chat function connects patients directly with designated HCP contacts, enabling patients or their caregivers to ask questions that relate to their situation at a given point in time. This provides HCPs with an invaluable window into the patient’s world, when otherwise they would have to rely on information reported after the event. The soon-to-be-added videoconferencing functionality will pave the way to further enhance remote care and introduces the potential for virtual clinics.
CHANGING THE PATIENTCLINICIAN DYNAMIC
Having pioneered the technology for pulmonary conditions, there is huge potential for expansion into other therapy areas. This technology forms part of the growing area of digital therapeutics (DTx), where the combination of technology and drug treatments delivers evidence based behavioural change and improved patient outcomes, enabling individuals or their caregivers to take greater control in preventing, managing and treating illness.
The optimism around DTx in recent years has been founded largely on its potential for changing the dynamic between HCPs and patients, particularly those with chronic conditions. This potential is now increasingly realised in commercial situations due to the alignment of a complex network of elements, including the drug and the device, hardware and software, data transfer and network connectivity, patient and HCP, and pharmaceutical companies and development partners.
As well as the continued introduction of innovative DTx products, these platforms are also being employed in applications such as clinical trials to return valuable data direct from the patients involved. In addition, the data on patient outcomes and clinical effectiveness held in DTx systems are used as the basis for value-based care contracts between HCPs and payers.
All these developments have been accelerated by the covid-19 pandemic, which has raised questions around the requirement for face-to-face interactions in more traditional healthcare settings, while also ushering in far greater acceptance of remote interactions via digital channels. Indeed, throughout 2020, the Digital Therapeutics Alliance, a non-profit association, petitioned international government bodies in Australia, Europe, the Middle East and North America to promote access to clinically validated digital therapeutic products during and after the pandemic.4
Even before covid-19, continued investment in DTx was expected to drive market value to a projected US$9 billion (£6.4 billion) by 2025.5 Perhaps more significantly, DTx has the potential to trigger a paradigm shift in the treatment of chronic conditions, driven by a robust, data led evidence base.
REFERENCES
- “Supported self-management for respiratory conditions in primary care”. PDF, The Primary Care Respiratory Society, 2017.
- Barry J, “Experiences of people with long-term conditions – what does GPPS data tell us?”. Ipsos.com, May 22, 2018.
- Tam A, Melvin E, Cushing A, Cohen J, Manice M, “Evaluating the BreatheSmart® Platform in Real World Settings to Assess the Use of Mobile Technology in Adult Asthma Patients”. Poster presentation. Accepted by the American Thoracic Society (ATS) and presented at the ATS Scientific Exhibition, San Diego, 2019.
- “DTA Petitions Countries For Digital Therapeutic Coverage”. Dtxalliance.org, June 18, 2020.
- “Digital Therapeutics Report: Latest DTx market trends and companies in growing digital health sector”. Businessinsider.com, December 15, 2020.

