Citation: Bordes-Picard F, Lamps J, Rode S, “Removing Clinical Trial Bias with Over-Encapsulation”. ONdrugDelivery, Issue 122 (Jul 2021), pp 4–7.
Frédérique Bordes-Picard, Julien Lamps and Stephen Rode discuss the considerations to take into account when using over-encapsulation to blind clinical trials, including the advantages of hydroxypropyl methylcellulose over gelatin as a material.
“Though simple in practical terms, over-encapsulating pharmaceuticals and blinding them for a study involves several unique operations that can introduce complexities that may be tough to manage effectively without support.”
During the preparation of clinical studies, best practice calls for identifying the method used to blind the dose form visually as early as possible in the drug development process. While there are many blinding options available, over-encapsulation remains the most popular method adopted by sponsors to meet regulatory requirements due to its relative simplicity.1
Double-blinding is the key to pharmaceutical trial robustness and study integrity.2 Beyond formulation and form, visually blinding trial doses becomes a critical factor in determining efficacy and therapeutic performance. A properly blinded study removes both investigator and patient bias caused by awareness of the drug’s source and suppresses potential placebo effects as well.
SIMPLE, YET COMPLEX IN PRACTICAL TERMS
Though simple in practical terms, over-encapsulating pharmaceuticals and blinding them for a study involves several unique operations that can introduce complexities that may be tough to manage effectively without support. Both the European Commission’s Volume 4 Good Manufacturing Practices Annex 13 and the US FDA’s 21 CFR Part 211 provide the regulatory framework for the use and qualification of comparative agents in clinical trials. Good manufacturing practice compliance requires:
- Provision of data to show that product quality has not been altered
- Justification of expiry dating
- Blinding that resists tampering and clearly reveals when tampering has occurred
- Rapid unblinding to identify the product in case of emergency.
Despite the relative simplicity of over-encapsulation, proper planning and careful execution are still fundamental to success – full consideration must be given to every detail from capsule colour and size selection, as well as engaging a well-trained team dedicated to the process.
PRIMARY OVER-ENCAPSULATION CONSIDERATIONS
It is important to select the appropriate components to support over-encapsulation of the trial tablet or capsule dose, as well as provide the means to prevent patients from discerning between investigational and control doses after receiving their clinical supply.
When the bioavailability of the investigational new drug is critical to determining efficacy, it is important that both the investigational and reference drug be encapsulated with the same capsule material so clear and appropriate comparisons and conclusions can be drawn. This is essential, for example, when similar in vitro dissolution profiles are called for in the clinical trial design.
SIZE MATTERS MORE THAN EVER
Once the trial dose form and formulation have been identified, determining what size of capsule shell is needed to properly blind each unit comes next. However, there are nuances to this. For example, although not completely necessary, Lonza Capsules and Health Ingredients (CHI) recommends from experience that efficiencies can be made if the dose being encapsulated does not protrude above the body of the shell when inserted (Figure 1). If the unit does not “sit” properly inside the body shell, issues can occur during the backfill process, which can increase waste, cause unnecessary downtime and, ultimately, raise cost.
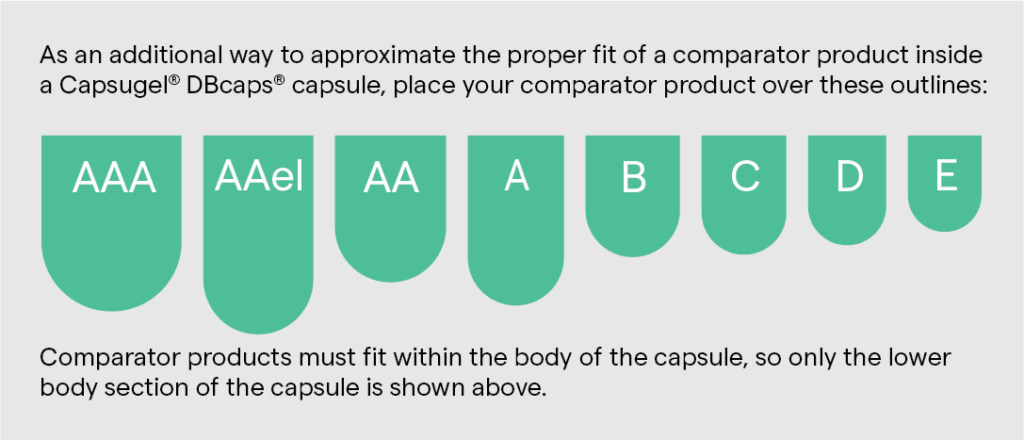
Figure 1: Over-encapsulation works best when the entirety of the dose fits inside the body of the capsule. [Image shown here is for illustration purposes only and is not to scale.]
“It is clear that capsule size is an extremely important detail to help assure trial supply dose compliance and blinding performance. Correctly specifying size requires data and input from all corners of drug development, trial design and administration.”
A study design might call for splitting tablets to fit them into the smaller capsule sizes to suit patient group requirements. However, splitting doses by physically breaking tablets is not a precise process and introduces variation. Regulators saw fit to mitigate this by prompting drug developers to address these issues during filling. However, that adds to the complexity and leads to greater demand for more flexible over-encapsulation solutions to fit more clinical supply dose forms.
It is clear that capsule size is an extremely important detail to help assure trial supply dose compliance and blinding performance. Correctly specifying size requires data and input from all corners of drug development, trial design and administration. This includes input from critical supply, equipment and fill-finish partners.
ELIMINATING TRIAL BIAS WITH COLOUR
First and foremost, the encapsulating capsule’s colour must completely obscure the enclosed dose form regardless of its colour. Ideally the colour and opacity of the capsule will hide any and all attributes that might give away the true identity of the contents. Anything that reveals which dose is which could impact patient compliance and trial data. For most applications, that means capsules for over-encapsulation are opaque and usually a different colour or colour combination to that of the dose being blinded.
It is certainly vital to select a capsule colour that blinds the dose and adds extra control to the study, but it is also important to assure the colour’s ingredients are accepted by regulators and meet dietary restrictions and source standards wherever the study is being conducted. Several countries have restrictions on particular colours or the total number of capsules.
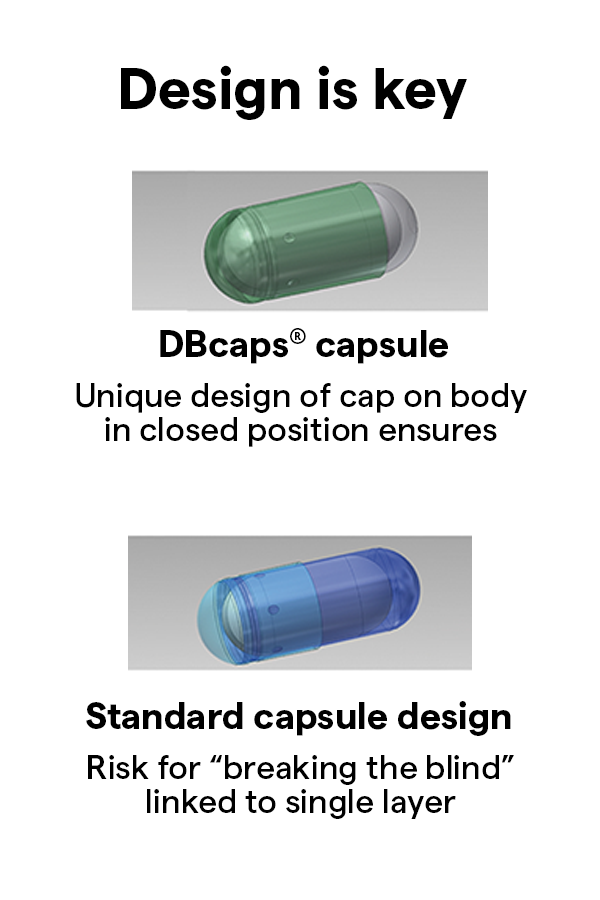
Figure 2: Lonza CHI’s DBcaps capsules double-layer the cap over the body which, combined with appropriate use of capsule colouring, ensures that the dose inside cannot be visually identified.
MOTION CONTROL EQUALS BLIND CONTROL
Over-encapsulation ensures blind control and study integrity because it completely hides which dose is being controlled (Figure 2). That extends to the “feel” and weight of blinded clinical supplies. For example, blinding a single small solid dose effectively usually requires a backfill of excipients to stop it from rattling around in the encapsulating capsule.
Of course, other control doses and placebos have to maintain the exact look and feel of every other dose being prescribed in the trial. If the rattle is not eliminated, the patient might possibly be able to identify if they are in the test or control group. Backfill can be avoided in certain cases, but only if a similar rattle between the doses can be maintained. Lastly, when selecting backfill excipients, it is preferable to choose one that is present in the dose form being blinded.
DO NOT FORGET TO CONSIDER DISSOLUTION AND STABILITY
Probably one of the more critical issues to consider when specifying an over-encapsulation capsule is its general compatibility with the trial and control doses, as well as any excipients. Considering the low solubility issues associated with today’s highly potent APIs, evaluating these factors is becoming more important than ever.
Among the most commonly used excipients for backfilling are microcrystalline cellulose and lactose monohydrate. While both are often used independently of one another and combined in blends, research has shown that combinations of the two can impact dissolution results. Depending on the grade of the material chosen, a lubricant, usually magnesium stearate, is added as part of the backfill formulation (usually less than 0.5%). However, not all grades of these two materials require lubrication, and adding the magnesium stearate is usually based on its presence in the formulation of the unit being encapsulated in the first place.
It is imperative to conduct dissolution profile and stability analyses early in development to verify that the material selected does not interfere with or create any bioavailability issues in the over-encapsulated dose form.
STORAGE AND SHELF-LIFE CONSIDERATIONS
Trial dose supply fill-finishers, among others, should also carefully consider the shelf life of encapsulating shells, along with similar storage-related concerns. For many sensitive potent formulations, storage and inventory control are extremely important to maintain the integrity of trial supplies during long trial cycles.
Extended periods of storage in dry conditions can turn capsules brittle and leave them prone to breaking, filling and quality issues. This is a quality assurance priority that should not be overlooked; close consultation with suppliers may reveal better-performing gelatin capsule materials or alternatives that deliver best-in-class performance and meet the industry’s increasing desire for cleaner-label ingredients.
Gelatin or HPMC? A Material Choice
While gelatin-based capsules offer traditional benefits and are backed up with data to prove compatibility, they do not meet clean-label requirements – i.e. being free from animal proteins or with colourings derived from natural sources.
Capsules based on hydroxypropyl methylcellulose (HPMC) show great potential for becoming the best-practice alternative to gelatin-based formulations, not only because of their provenance but their performance as well. Further benefits include circumventing the regulatory burden of working with animal derivatives and their global market acceptance for multi-centre studies.
HPMC-based capsules are widely preferred in clinical trials, and for many investigational new molecular entities (NMEs), because they have the added flexibility to accommodate a vast array of drug products and formulations. With many potent NMEs in development, the challenges related to deploying APIs in gelatin-based capsules are contributing to a shift towards the use of HPMC-based capsules. Issues with cross-linking reactions and difficulty containing hydroscopic APIs top the list of these challenges.
Benefits of HPMC-Based Capsules
HPMC-based capsules offer a higher moisture tolerance compared with their gelatin-based counterparts, which helps to stabilise formulations and to mitigate the challenges associated with APIs and excipients that are incompatible with gelatin. Furthermore, HPMC-based capsules can boast a wider range of moisture tolerance and can withstand a wider range of temperature variation and fluctuation in storage and transit, meaning there is less chance of the capsule becoming brittle or breaking.
CONCLUSION
Over-encapsulation is one of the simplest solutions for blinding solid oral dosages in comparative clinical trials. Compatibility with the trial API must be the highest priority when investigating options for over-encapsulation. Dissolution, diffusion and stability studies are essential elements of selection and therapeutic performance. Furthermore, patient-centricity is increasingly informing selection and specifying criteria, leading to the development of innovative clean-label HPMC-based capsules compatible with vegetarian and vegan lifestyles. Of the many blinding options available, the over-encapsulation method using products such as DBcaps from Lonza CHI is one of the most commonly applied options for efficiently controlling and blinding oral solid doses in clinical trials today.
REFERENCES
- Back-Moore K, “Qualification Strategies for Blinded Comparators: One Company’s Perspective”. Pharmaceutical Outsourcing, Mar 2011.
- Crisp A, “Blinding in pharmaceutical clinical trials: An overview of points to consider”. Contemp Clin Trials, 2015, Vol 43, pp 155–163.

