To Issue 182
Citation: Bruno G, Buerdel S, “Frictionless Engagement: How Gx InMonit™ can Simplify Self-Injection and Strengthens Patient Adherence”. ONdrugDelivery, Issue 182 (Jan 2026), pp 78–82.
Visit Gerresheimer at Pharmapack Paris! – Stand 4G36
Dr Giacomo Bruno and Simon Buerdel consider the causes of patient non-adherence and its subsequent effects on healthcare systems, going on to present the solutions created by Gerresheimer to address the patient experience across treatment types.
Digital health interventions have emerged as a promising strategy for improving patient drug adherence in self-administration.1–5 The combination of mobile health apps and connected devices can remind, motivate and monitor patients. For example, a recent trial investigating severe mental illness showed that a digital medication system increased the proportion of patients adhering to treatment from 21% to 78%, helping to reduce complications and hospitalisations.1,6
However, creating a closed loop with Bluetooth-based connected devices remains limited due to technological limitations, security and poor user experience.7–9 Additionally, traditional app-based solutions can suffer from poor patient engagement and retention.10,11 Some patients are reluctant to download yet another smartphone app to manage their therapy or to go through complex device setups, leading to high dropout rates.12 Thus the critical challenge is to deliver a holistic adherence support solution that can be integrated with minimal friction into the everyday routines of patients.
CHALLENGES OF SUBCUTANEOUS SELF-ADMINISTRATION
According to a WHO report, non-adherence can account for up to 50% of treatment failures, around 125,000 deaths and up to 25% of hospitalisations each year in the US.13 First understood over 20 years ago, recent studies are still looking for a paradigm shift to address the issue of non-adherence.14–16 The consequences are significant – worsened clinical outcomes, increased hospitalisation rates, avoidable disease progression and a substantial waste of healthcare resources.14
Although at-home self-administration with an autoinjector can enhance patient independence while reducing the burden on healthcare systems, it can also add further procedural complexity. Outside of clinical supervision, patients must manage the entire sequence themselves – preparing the device, selecting the injection site, performing the injection and confirming completion. This often heightens anxiety and uncertainty, introducing a cognitive and emotional burden that may negatively affect confidence and consistency.17
Notable challenges of self-administration include:
- Patient Discomfort: High injection forces can increase discomfort, which may impact adherence and require engineering solutions.18
- Adherence: Extended injection times and multistep handling may impact adherence, particularly among patients with limited dexterity.
- Efficacy: Complete dosing within an acceptable timeframe is essential for therapeutic performance and is especially challenging for high-viscosity biologic formulations.19
- Engagement with Digital Applications: Despite strong evidence, real-world adoption often stalls due to cumbersome onboarding processes and difficulty scaling engagement beyond controlled pilot studies.20
- Emotional Considerations: Many individuals experience fear of pain, hesitation about performing an injection correctly (particularly with expensive medications) or uncertainty about whether the full dose has been delivered.17 Others may feel overwhelmed by instructions, concerned about side effects or unsure how to integrate injections into their lives.
- Lack of Real-World Evidence: With self-administration outside of a healthcare environment, pharma companies and healthcare providers (HCPs) lack objective insights into patient use, adherence and adverse events.21
- Instructions for Use (IFU) Unread or Misunderstood: Studies have shown that less than a third of patients read and understand a drug’s IFU – a particular concern for long-term therapies.22,23
Together, these factors highlight the need for solutions that ease cognitive load, support patients before, during and after self-injection, and provide guidance in a way that feels intuitive, familiar and effortless.
OVERCOMING THE CHALLENGES OF SUBCUTANEOUS SELF-ADMINISTRATION
User-Centric Autoinjector Design
The Gx Inbeneo® autoinjector is designed to overcome many of the usability, emotional and procedural challenges associated with self-administration. Its cartridge-based architecture and optimised double-ended needle system enable highly viscous formulations to be delivered in less time. Intuitive handling with simple two-step administration and a unique visual indicator supports usability and injection tracking.24
While such an innovative, user-centric autoinjector design concept already represents a significant step, there are additional factors that affect the patient before and after the injection, such as psychological blocks, forgetfulness, side effects and pain management. A survey conducted by Gerresheimer with a cohort of 57 participants self-injecting a prescribed medicine for a long-term condition reported that confidence substantially increased over time. However, the data also indicated a persistent subgroup with low confidence: despite overall improvement, approximately 16% of participants continued to rate themselves as unsure or very unsure when injecting.

Figure 1: The Gx InMonit smart add-on assembled on top of a 3 mL Gx Inbeneo autoinjector.
Patient Guidance at the Moment of Injection
To address potential patient anxiety with self-injection, Gerresheimer has developed Gx InMonit, a reusable smart add-on designed to be mounted on top of an autoinjector such as the Gx Inbeneo (Figure 1). It features a large, high-contrast, easy-to-read AMOLED display that guides the patient step-by-step through injection preparation, initiation, progress and confirmation of completion. Real-time detection of injection start, stop, premature removal or potential injection failure using motion sensors provides the reassurance that many patients seek.
Gx InMonit also incorporates temperature monitoring and verification of the device, drug and dose by scanning a near-field communication (NFC) tag under the label of the autoinjector. This combination of features can reduce uncertainty and ensure that patients conduct injections with authentic devices correctly and in alignment with the prescribed care plan. The Gx InMonit device needs no additional user actions such as pairing, app installation or manual data upload; data are transmitted automatically to the cloud through its embedded cellular module, allowing patients to remain fully focused on their therapy.
“GERRESHEIMER IS DEVELOPING
AN AI-DRIVEN, TWO-WAY MESSAGING APPLICATION, GX ADHERALINK, TO COMPLEMENT GX INMONIT AND PROVIDE A COMBINED ECOSYSTEM THAT FURTHER ENHANCES PATIENT SUPPORT.”
Agentic AI-Driven Actionable Patient Support
While Gx InMonit provides guidance and captures accurate data at the point of self-administration, patients can also benefit from support before and after injections (Figure 2). Gerresheimer is developing an artificial intelligence (AI)-driven, two-way messaging application, Gx AdheraLink™, to complement Gx InMonit and provide a combined ecosystem that further enhances patient support.
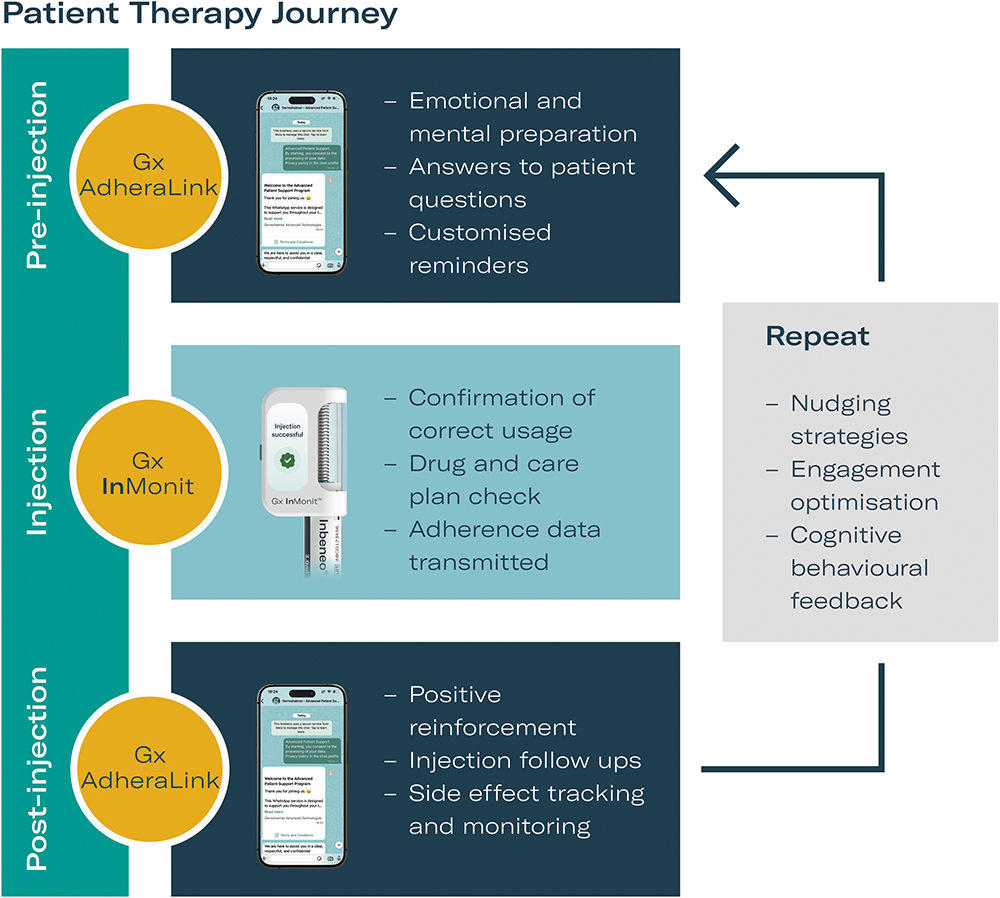
Figure 2: Benefits for patients and pharma of the Gx InMonit combined ecosystem providing a closed-loop patient support strategy.
Before a scheduled injection, Gx AdheraLink can provide timely reminders and gentle prompts, also known as nudges, which helps patients to mentally prepare for the upcoming injection and may, in turn, reduce anxiety and strengthen routine formation. Such methods have been shown to significantly improve patients’ self-management for chronic conditions.25 After the injection, the system follows up with positive reinforcement in the form of encouraging messages, based on cognitive behavioural therapy methods. It subtly collects information about the injection experience, injection location, pain level, overall experience and side effects, which can then be used for reporting and monitoring by an HCP.
To achieve this support, Gx AdheraLink uses agentic AI that interacts with patients on an instant messaging application, such as WhatsApp or iMessage, that most will already have installed on their phones. By employing a preferred app that is already integrated into a patient’s everyday life, Gx AdheraLink can create two-way communications that are personalised, smart and immediate. User friction is reduced, as there is no need to install a new app, learn a new interface or navigate additional accounts. The solution also offers the possibility of using multimedia-rich conversations such as a video-based IFU.
Together, Gx InMonit and Gx AdheraLink form a unified ecosystem designed to reduce patient burden, improve engagement and support therapy outcomes with objective data. As the two solutions operate across the full therapy journey, they create a dynamic feedback loop that transforms them into a self-regulated system. Each interaction generates behavioural signals that feed back into the platform, allowing different nudging and engagement strategies to be evaluated. Those that are most effective can then be progressively reinforced to create a tailored approach for each patient. Over time the platform evolves into a personalised cognitive-behavioural companion: it reinforces correct patient actions, gradually builds confidence and lays the groundwork for effective future injections.
CONFIRMATION OF PATIENT NEED AND INTEREST
Qualitative User Study Reveals Pain Points
The development of any Gerresheimer solution starts with gathering input from users and stakeholders. In this case, the first step was to conduct qualitative user research with 12 US patients dealing with various autoimmune diseases. The user research was divided into two cohorts with six patients each. The goal was to understand the user’s perspective when self-administering recurring monthly injections with an autoinjector, in order to evaluate the utility of the Gx InMonit add-on device and Gx AdheraLink digital support.
Participants reported anxiety towards self-injecting and fear of making mistakes with drugs, even when this has been their routine for several years. Subjective feedback on a potential add-on device highlighted the value of real-time guidance, sensing the temperature of the injection device and additional information on delivery success or error. The interview with the first cohort revealed that 83% of the patients believed that an add-on device and an app could increase their confidence when self-injecting. All the participants from the second cohort rated a digital companion app as useful (33%) or very useful (67%) for reminders, injection and symptom tracking, guidance on injection errors and communication with HCPs.
The study revealed that an add-on and companion solution complement each other, highlighting that users place strong value on receiving reminders for injection schedules, feedback on drug temperature, and additional audible and visual real-time feedback on injection progress that align with existing self-management techniques.
Gathering Deeper User Insights
After the initial assessment of challenges faced by patients, a further survey was implemented. Of the 90 respondents from the US who self-injected regularly to treat conditions other than diabetes and weight management, 83% expressed a desire for a digital solution that could support their therapy journey. However, a solution capable of tracking injections, sending reminders and providing drug information, was being used by less than a quarter (24%) of the interviewed population (Figure 3). When asked if they would use an AI-driven medical assistant, over 80% of the respondents said yes (Figure 3). This survey revealed a positive attitude towards a smart digital support solution among participants and highlighted that the use of AI was also viewed positively.
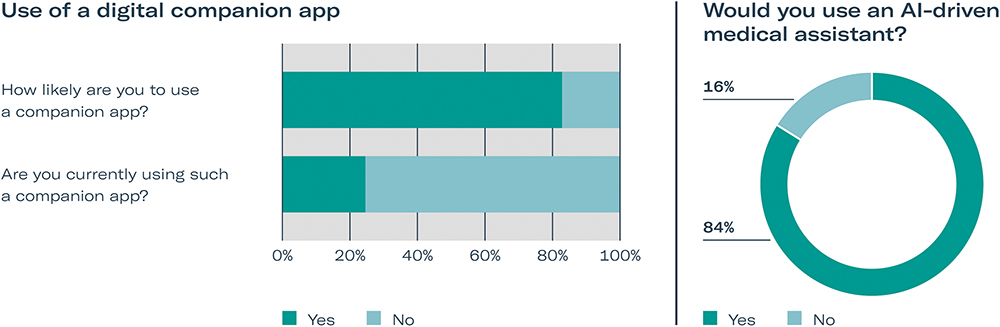
Figure 3: Interest in a digital solution to help manage therapy from 90 respondents to a user survey of patients regularly performing self-injections for chronic conditions (excluded diabetes and weight management).
Based on user research and market evaluation, Gerresheimer developed the ecosystem of Gx InMonit and Gx AdheraLink. At this stage of development, a third user research study was conducted with 57 individuals with similar profiles and injection frequencies, ranging from once per week to twice per year. The response to such a combined solution was overwhelmingly positive: 90% would consider using a connected digital companion to support their therapy journey. When asked how they would prefer to receive this support, the majority (74%) selected instant messaging as their preferred channel, far surpassing the interest in a dedicated app (14%) or a web-based application (12%), as shown in Figure 4. Notably, approximately 70% of participants also believed that such a solution would help them emotionally and make it easier to take their medication more consistently.
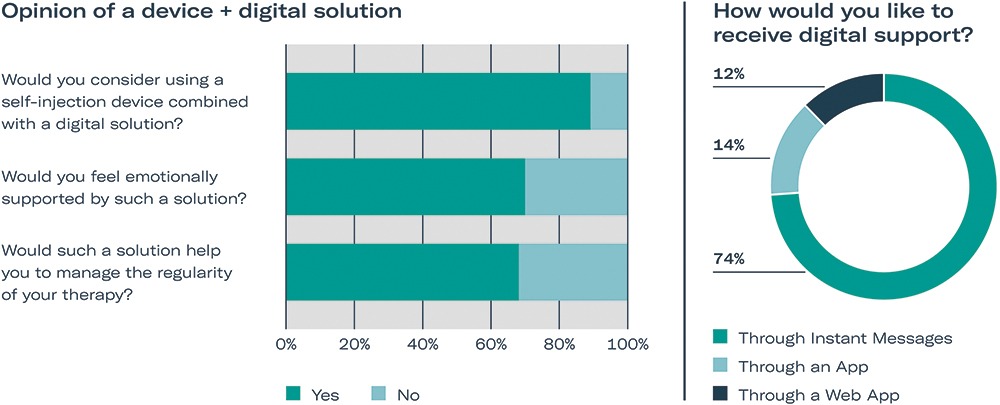
Figure 4: Interest in a device + digital solution from 90 respondents to a user survey of patients regularly performing self-injections for chronic conditions (excluding diabetes and weight management).
BENEFITS OF THE COMBINED GERRESHEIMER ECOSYSTEM FOR STAKEHOLDERS
Addressing Non-Adherence
The Gx InMonit–Gx AdheraLink ecosystem tackles the core problem of non-adherence by supporting patients before, during and after each injection, with the goal of achieving more consistent dosing, higher therapy persistence and optimal therapy outcomes. For pharma, this could translate into stronger therapeutic performance and more reliable real-world evidence.
Scalability Across Markets
The solution is easy to deploy globally because Gx AdheraLink uses messaging apps already installed on patients’ phones and Gx InMonit functions as a reusable add-on, without requiring additional gateways or dedicated apps.
Value-Based Healthcare Models for HCPs
Gx InMonit gives clinicians direct visibility into patient behaviour without adding extra workload, making it easy to identify missed or incomplete doses and intervene early on. Gx AdheraLink enriches this view with patient-reported information, such as pain, fatigue or side effects, which supports more personalised clinical decisions. This combined insight helps strengthen continuity of care, especially for chronic conditions where consistent self-administration is essential.
Traceability and Real-World Evidence
Gx InMonit generates objective real-world evidence through automated, reliable injection data, supporting pharmacovigilance, value-based care models and outcome analysis. Integrated drug-identification and anti-counterfeiting capabilities ensure that medication type, batch number and expiry date are captured and verified securely, enhancing supply chain integrity and enabling advanced monitoring strategies.
CONCLUSION
Improving adherence is a multifaceted endeavour requiring innovation in both human factors and technology. The Gx Inbeneo autoinjector from Gerresheimer, combined with a smart and connected add-on, demonstrates a promising model of “digital + device” synergy that benefits all stakeholders: patients could receive a patient-focused treatment experience that potentially leads to a better outcome, while pharma could gather more relevant evidence to prove the value of their therapies. Such an integrated approach transforms the act of self-injection from a solitary, often uncertain task into a guided, connected experience that integrates the patient into a supportive network. As healthcare systems globally continue shifting towards outcome-based models, connectivity solutions help to confirm that medications can deliver on their promised real-world benefits.
REFERENCES
- Zhou J et al, “Randomized clinical trial of a digital medication system to enhance adherence in patients with severe mental disorders”. npj Digital Medicine, 2025, Vol 88(1), p 333.
- Lanke V et al, “Evaluating the Effectiveness of Mobile Apps on Medication Adherence for Chronic Conditions: Systematic Review and Meta-Analysis”. JMIR, 2024, Vol 27, art e60822.
- “Komodo Health analysis finds Medisafe’s digital drug companions improve medication adherence and extends persistence”. PDF, Medisafe, 2022.
- “IQVIA Study Proves Medisafe Digital Companion”. PDF, Medisafe, 2019.
- “IQVIA Study Proves Medisafe Digital Companion”. PDF, Medisafe, 2020.
- Kim SK et al, “Effectiveness of Mobile Health Intervention in Medication Adherence: a Systematic Review and Meta-Analysis”. J Med Syst, 2025, Vol 49(1), p 13.
- Lonzetta AM et al, “Security Vulnerabilities in Bluetooth Technology as Used in IoT”. J Sens Actuator Netw, 2018, Vol 7(3), p 28.
- “Seventy-Six Percent of People With Diabetes Have Issues Transmitting Their Reading Using Bluetooth® Glucose Meters”. Business Wire, Nov 2024.
- Pidgeon A, “Smart Enough: Designing Drug Delivery Devices that Put Patients First”. ONdrugDelivery, Issue 174 (Jun 2025), pp 12–15.
- Helander E et al, “Factors related to sustained use of a free mobile app for dietary self-monitoring with photography and peer feedback: retrospective cohort study”. J Med Internet Res, 2014, Vol 16(4), art e109.
- Wang Y et al, “A systematic review of application and effectiveness of mHealth interventions for obesity and diabetes treatment and self-management”. Adv Nutr, 2017, Vol 8(3), pp 449–462.
- Meyerowitz-Katz G et al, “Rates of Attrition and Dropout in App-Based Interventions for Chronic Disease: Systematic Review and Meta-Analysis”. J Med Internet Res, 2020, Vol 22(9), art e20283.
- “Adherence to long-term therapies: evidence for action”. World Health Organization, 2003.
- Bosworth HB et al, “Medication Adherence: A Call for Action”. Am Heart J, 2011, Vol 162(3), pp 412–424.
- Kim J et al, “Medication Adherence: The Elephant in the Room”. US Pharmacist, 2018, Vol 43(1), pp 30–34.
- Kardas P et al, “Medication non-adherence: reflecting on two decades since WHO adherence report and setting goals for the next twenty years”. Front Pharmacol, 2024, Vol 15, art 1444012.
- Coyne M, “Impact of Routines and Rituals on Burden of Treatment, Patient Training, Cognitive Load, and Anxiety in Self-Injected Biologic Therapy”. Patient Prefer Adherence, 2022, Vol 16, pp 2593–2607.
- Pager A, Duinat B, Alves B, “Shorter Needles with Thinner Walls are Set to Improve the Injection Experience in Chronic Care”. ONdrugDelivery Magazine, Issue 107 (May 2020), pp 37–42
- Mathaes R et al, “Subcutaneous Injection Volume of Biopharmaceuticals-Pushing the Boundaries,” J Pharm Sci, 2016, Vol 105(8), pp 2255–2259.
- ‘’Pharmaceutical Mobile App Usage and Engagement Strategies”. PDF, IntuitionLabs, Jan 2025.
- Dunbar-Jacob J and Zhao J, “Medication Adherence Measurement in Chronic Diseases: A State-of-the-Art Review of the Literature”. Nurs. Rep, 2025, Vol 15(10), p 370.
- Raynor DK et al, “How do patients use medicine information leaflets in the UK?”. IJPP, 2007, Vol 15(3), pp 209–218.
- “Disposing of the paper leaflet: The challenges with Patient Information Leaflets”. Blog, Datapharm, Mar 2023.
- Primavessy D, Saaler-Reinhardt S, Maksymowicz K, Stockton M, “Gx Inbeneo® – Developing an Autoinjector that Responds to the Challenges of Biologics”. ONdrugDelivery, Issue 152 (Oct 2023), pp 32–36.
- Möllenkamp M et al, “The effectiveness of nudges in improving the self-management of patients with chronic diseases: A systematic literature review”. Health Policy, 2019, Vol 123(12), pp 1199–1209.

