To Issue 152
Citation: DeSalvo D, “Identifying and Overcoming the Challenges of Injectable Combination Product Evolution”. ONdrugDelivery, Issue 152 (Oct 2023), pp 14–17.
David DeSalvo considers some potential challenges that the rapid evolution of autoinjectors (and combination product injectables in general) raises, along with how the industry can successfully address this cycle of reinvention.
Since the creation of the rescue autoinjector in 1959, these drug-device combination products have evolved significantly in functionality, capabilities and popularity. The transition of autoinjectors from emergency-use military devices to becoming an at-home therapeutic delivery method has made them a part of many people’s daily lives, and the sustained preference for these devices is based primarily on their ease of at-home use and the reduced burden they offer for all stakeholders. This popularity has helped propel innovation for both the devices and the drugs they contain, which means rapid adjustment continues to be necessary on the part of patients, sponsors, contract development and manufacturing organisations (CDMOs) and everyone using or creating these products.
“Weekly injections enable high-production volumes, which, in turn, bring down the per-unit cost for the pharmaceutical company.”
A critical benefit offered by autoinjectors and related devices is their at-home use, which provides all-around savings in time and costs. For patients who need, for example, weekly injections, this means that there is no need to routinely schedule appointments, travel to the doctor’s office, wait to be seen, get the injection and go home. Having a device that the patient can safely and effectively operate delivered directly to them means that they can avoid the potential disruption to their day, lost family or work time and wasted time on the road and in the office, while simultaneously saving money on transportation costs (and, in doing so, cutting emissions). In addition, physicians and other qualified practitioners can focus on providing treatment options for more patients, possibly reaping financial benefits as a result. These factors are all key to the continuing push towards new patient solutions that still offer similar benefits.
THE PROMISE AND THE PITFALLS
As with any technology, the ongoing evolution of these devices brings plenty of potential challenges with it (Figure 1). While many of these nascent innovations are still finding their footing, furthering their development while keeping a critical eye open for identifiable trouble spots can help counter those difficulties head-on, saving headaches down the road.
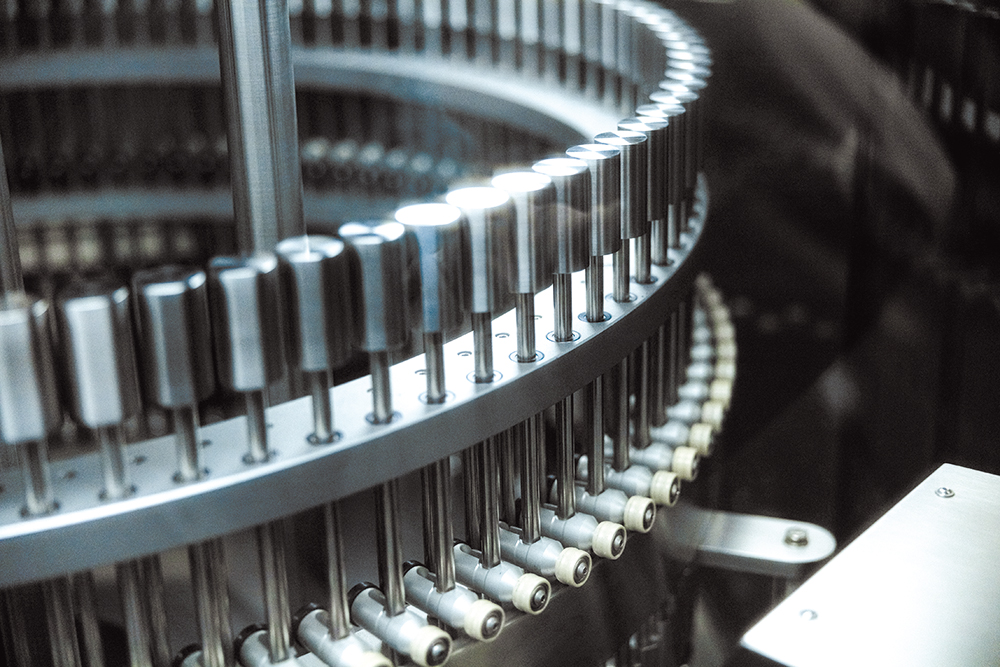
Figure 1: Technology is quickly becoming an expected component of combination products, bringing a specific set of challenges with it.
Long-Acting Injectables
For decades, long-acting injectables (LAIs) were associated primarily with antipsychotics to aid patients with schizophrenia who struggled with adherence to oral formulations, but the same principles are now being applied more regularly to other therapeutic areas.1 These drugs are formulated for controlled release over an extended period, promising increased adherence and additional opportunities for time savings for patients and healthcare providers, such as those previously discussed, even in clinical settings.2 The move of LAIs to at-home delivery could increase those benefits on all sides, but that potential comes with its own set of risks.
The ongoing desire to extend the timeline from one injection a week to one every two weeks, or even one a month or more, may begin to impact the ability of the patient to use their device correctly. The lower the frequency of injection, the more deterioration in training is likely to occur. With that comes a greater potential for injection and other user errors that could impact the efficacy of the therapy, particularly when the next dose may not be administered for weeks. The possibility of training degradation must be considered when evaluating and planning the ease of administration and the availability of instruction to ensure that the LAI achieves its goal.
“The original limitations of handheld autoinjectors have been disproven, but caution should still be exercised when pushing their limits.”
Given the increased payload required for these formulations to release over extended periods, the need for greater volumes may necessitate delivery in the form of wearables in place of hand-held autoinjectors. While these devices can help correct some training issues in terms of delivery, their complexity raises a different array of related problems. Patients who may have difficulty retaining their training with autoinjectors are no more likely to recall the right steps for more complicated devices that integrate injectables with electronics. In addition, wearables raise specific challenges due to the duration of use, including becoming dislodged or negatively impacting user compliance due to discomfort, among other issues. As with autoinjectors, ease of use and instructions are vital to ensuring that these devices work as planned for the patient.
On a more practical note, the savings patients achieve from at-home administration could easily be offset by the cost of LAIs. Weekly injections enable high-production volumes, which, in turn, bring down the per-unit cost for the pharmaceutical company. Once the rate of injection slows to once a month or once a quarter, production volume drops and the cost per unit soars. Furthermore, devices that deliver large volumes of medicine over longer periods tend to be significantly more complex and disproportionately more expensive to produce. To determine the effect on the patient, the price for a monthly LAI should be compared with the cost for a month’s worth of its weekly counterpart. With the change in production costs, the potential for them to be equitable needs to be considered. Given that device quality should remain uncompromised, the financial burden for the payers and patients must be considered when extending the time between doses.
Technical Advances

Figure 2: When creating a technologically advanced injectable product, it is important to ask whether there is adequate benefit to the patient to offset the potential problems associated with the upgrades.
Information technology is quickly becoming an expected component of combination products, which, as discussed, brings with it a specific set of challenges. These devices can, however, also offer several benefits, including tracking of dose adherence and therapeutic response through connected devices. Some wearable smart injectables can even ensure that the device is being used properly.
While the complexity of these products and the associated potential for higher pricing are both possible issues for patients, privacy and payer problems are also concerns. Built-in security for these systems may be high (and highly regulated), but no technology is impenetrable, which is a risk when dealing with protected health information. On the payer side of the equation, there is the risk of denial if there is an electronically tracked adherence issue or the benefit is not deemed significant or fast enough to warrant the price tag.
When creating a technologically advanced injectable product, it is important to ask whether there is adequate benefit to the patient to offset the possible problems associated with the upgrades. If the downsides outweigh the upsides, it is necessary to consider whether the technology is necessary or simply nice to have (Figure 2).
Increased Expectations
While the initial consideration of a 1 mL maximum dosage for subcutaneous injection held for years, the boundaries have been shifting in a manner that resembles one-upmanship. The theory had long been that larger doses would be delivered by wearables or other devices, but the initial push in autoinjectors to 1.2 and 1.5 mL was well tolerated, which led to a push to 2 mL, then 3 mL, and now we have seen launches of 5 mL devices for subcutaneous delivery.
The original limitations of handheld autoinjectors have been disproven, but caution should still be exercised when pushing their limits. As discussed in a previous article, among the issues to consider when creating a large-dose autoinjector are tolerability (including an increase in pain, adverse events, injection-site reactions and leakage), the suitability of the device for self-administration and pharmacokinetic equivalence with other options.3 If there are increased risks for the patient or better options already available, the reward for increasing the dosage is potentially outweighed by the consequences.
One alternative to these increased volumes is packing more of the API into a smaller dosage, which will often increase the viscosity. Along with some of the same issues already discussed, this switch often requires a significant reconfiguration of the device itself. A spring-driven device, for example, is limited by the amount of liquid that it can push through a very small needle, and when the drug being administered is thickened, there is a commensurate need for more power from the autoinjector. The easiest solution in this case is increasing the size of the needle, but this requires a determination of whether patient comfort or flow characteristic is the more important element. This, in turn, leads to the debate over whether you should adjust the formulation development, the device development or both – a decision made more complex by the fact that they are often handled by separate, unaffiliated organisations and separated by months, or even years, within an overall drug development programme. There is no easy answer in this instance, but consideration of both basic device effectiveness and the ability of patients to operate it and adhere to their dosing regimen must be made.
TRANSFORMING TOMORROW
Knowing where the challenges are in the ongoing evolution of autoinjectors and other injectable combination products makes it possible prepare in advance for what is to come.
While there is no way to future-proof against the forming tides of tomorrow, there is an opportunity to avoid being swept away by them. One place to start is with early and close collaboration with partners; forging solid relationships between sponsors, CDMOs and other stakeholders is key to creating a comfortable working relationship and ensuring that all parties are involved in projects from as early in the project as possible. This can help to identify the potential issues so that they can be addressed immediately, saving time and money while ensuring the best chance of creating an optimal product. While it may seem premature to engage a device partner during formulation, these devices are called “combination products” for a reason. There is wisdom to be gleaned from all sides in terms of how to develop the right product for the intended use. Along with determining that the formulation that fits the device, early and consistent collaboration allows for the syncing of reliability and durability expectations, as well as acceptable cost per dose or device. By bringing the two halves together from the beginning, it is possible to ensure that a truly cohesive product is created based on the respective expertise on each side of the equation.

Figure 3: Injectable combination products are already complex, and that complexity continues to increase.
What the future holds for autoinjectors and other at-home injectables is an open question. Should there eventually be a move from a weekly dose to an annual dose, does it simply make more sense to return to the doctor’s office instead of asking the patient to recall proper administration from a year ago? Do devices become so complex that each patient needs a dedicated technical support person working alongside their physician (Figure 3)? If viscosity continues increasing, how large a needle will patients agree to endure? The key to ensuring that these questions are answered before they become reality is communication. Injectable combination products are already complex, and if that complexity continues to increase, true co-operation and discussion among the experts developing them is the only way to ensure that the products delivered to patients live up to their promise.
REFERENCES
- Brissos S et al, “The role of longacting injectable antipsychotics in schizophrenia: A critical appraisal”. Ther Adv Psychopharmacol, 2014, Vol 4(5), pp 198–219.
- O’Brien M et al, “Challenges and opportunities in the development of complex generic long-acting injectable drug products.” J Control Release, 2021, Vol 336, pp 144–158.
- Schneider A et al, “Autoinjectors for large-volume subcutaneous drug delivery: A review of current research and future directions.” Expert Opin Drug Deliv, 2023, Vol 20(6), pp 815–830.

