To Issue 139
Citation: Seeney P, Winkworth P, Nelson C, “Making Sustainability by Design the Lintel of Sustainable Inhaler Development”. ONdrugDelivery, Issue 139 (Oct/Nov 2022), pp 50–55.
Phil Seeney, Philip Winkworth and Craig Nelson provide an insight into sustainability developments in the pharmaceutical industry, with a focus on inhalables.
Climate change and sustainability have become important drivers for much of what we do in our daily lives and in selecting the products we, as consumers, use. Government policy, international legislation and company strategies all attempt to address the sustainability challenge. Products such as medical devices, including inhalers, are no exception, with recent regulatory and advisory guidelines driving change, including:
- Targets/policies emerging in healthcare systems, such as UK NHS England targets1 encouraging a switch to more environmentally friendly alternatives
- Earlier, similar guidance from NICE,2 the MHRA consultation on new future device regulation looking at sustainability3, and the emergence of the Sustainable Medicines Partnership4 also encourage change
“The pharmaceutical industry is currently addressing the sustainability issue with a range of initiatives ahead of actual legislation being in place.”
While currently there is no definitive “environmental” legislation that covers inhalers and other medical devices, we can anticipate it will not be long before legislation drives change or economics force change via national and supranational bodies, whose policies will impact the costs of material supply and demand (thereby cost). We have seen moves like these before, with the Montreal Protocol5 limiting the use of chlorofluorocarbons (CFCs), which led to significantly increased costs for CFCs and, ultimately, a forced move by pharma to hydrofluoroalkanes (HFAs) across the industry.6 With new legislation to protect the environment appearing inevitable, the impact can be limited by considering the apocryphal Benjamin Franklin saying, “By failing to prepare you are preparing to fail.” Acting early will become paramount to achieve a commercial and sustainable advantage or, indeed, to survive.
The pharmaceutical industry is currently addressing the sustainability issue with a range of initiatives ahead of actual legislation being in place, and this can be demonstrated by companies such as Chiesi, GSK, AstraZeneca, Takeda, Novo Nordisk and Merck & Co investigating and analysing their sustainability profiles and environmental impact at a company, supplier and product level.7 This article mainly considers devices and their manufacture. However, it is increasingly seen that pharma companies are taking an even wider holistic approach to include the sustainability aspect of the manufacture and supply of the drug product (which, although not addressed here, follows similar principles of assessment).
Inhalers and inhaled products are nominally very small contributors to the overall climate budget (0.05% of all greenhouse gas emissions)8 but significant in the specific sustainability picture for suppliers (e.g. GSK – 32% of its carbon footprint)8 and healthcare providers like the NHS (4% of the entire NHS carbon footprint).6,9
“Companies will be challenged to deliver not only better healthcare to patients but also healthier solutions for the planet.”
Current inhalers present a number of issues from an environmental perspective, including the propellants used in pressurised metered dose inhalers (pMDIs) and the polymers used in dry powder inhaler (DPI) products, both of which are disposed of after a month of use. Inhalers, with their long-established design and delivery of essential therapeutics, represent a challenge for achieving sustainability targets. With the pressures from national policy, internally and from the wider public, a pre-emptive and rapid move towards more sustainable devices would seem prudent before legislation potentially enforces it on the wider landscape and potentially unprepared suppliers. However, there is not a universal inhaler that suits every patient and not all drugs are available in every type of inhaler in use. Inhalers do, therefore, present a distinct challenge here, given their current varied design(s) and the options available to prescribers.
A number of recycling schemes and initiatives have been piloted in the past with little benefit and the NHS has no plans for a national recycling scheme.10 However, to encourage the move to a more sustainable future, there is clearly a need (and therefore an opportunity) to make a more fundamental change – a core change in culture – by designing new devices to better enable recycling and address the needs of patients and the planet. Companies will be challenged to deliver not only better healthcare to patients but also healthier solutions for the planet. Patients are, after all, consumers and, as such, receive constant stimulation to purchase and use more sustainable products.
Consumer products are going through a sustainability revolution and many companies are building brand loyalty and growing market share based on their “sustainability credentials” and awareness of how their activities are impacting the planet. Eventually, patients will expect and even demand environmentally sustainable medicines and will expect to be given a choice. Of course, as industry and healthcare professionals, we have a duty of care to ensure that patients are not pressured to change medication on environmental grounds alone; if there is a risk the alternative product puts the patient at increased health risk (either through its different drug or via a different delivery mechanism the patient cannot handle), then a change cannot be justified. Thus, the opportunity of starting from a blank sheet of paper and building in sustainability by design to create a new breed of inhalers increasingly seems the only viable option to achieve long-term sustainability and patient-care goals. Such an approach will enable companies to keep ahead of future legislation and provide potential competitive advantage, but in a way that does not compromise product performance or put the patient at increased risk. Quality by design (QbD) is already part of the culture for many drug delivery companies, but building in sustainability requirements (sustainability by design (SbD)) as a critical element of the quality management system (QMS) will mean that emerging designs will provide quality, maintain performance for patients, achieve sustainability goals and be better for the planet.
There are several ways to achieve such a redesign. Such an approach will demand that we explore these emerging critical elements in addition to the delivery performance and human factors that currently drive device design. PA Consulting’s approach is to consider the technological, design and (importantly) the planetary health aspects of future platforms and products. By focusing on these three pillars and incorporating learnings from the consumer and manufacturing sectors, we can design a new generation of inhalers fit for purpose, fit for the planet and fit for more demanding patients.
“The long-term solution is to design the next universal platform for liquid inhaled drugs that can be adopted by the majority of pharmaceutical companies.”
TECHNOLOGY
When considering technology, if we start from first principles, understanding how a formulation can be aerosolised may offer a route to a more sustainable product. Can we pick a more sustainable technology or method of delivery? Can we use alternative aerosolisation technologies that can deliver longer inhaler use and more doses over the life of the device, reducing the cost per dose – both financially and environmentally? Can we avoid the use of environmentally unfriendly propellants completely for liquid formulations? Of course, the answer to the latter question is “yes, potentially”, since solutions already exist – but we can do more and, ultimately, create products that can be as cost effective as pMDIs without using environmentally damaging propellants. Given there is a wide range of alternative methods to aerosolise liquid formulations (Figure 1), there are potential alternatives to using propellants.
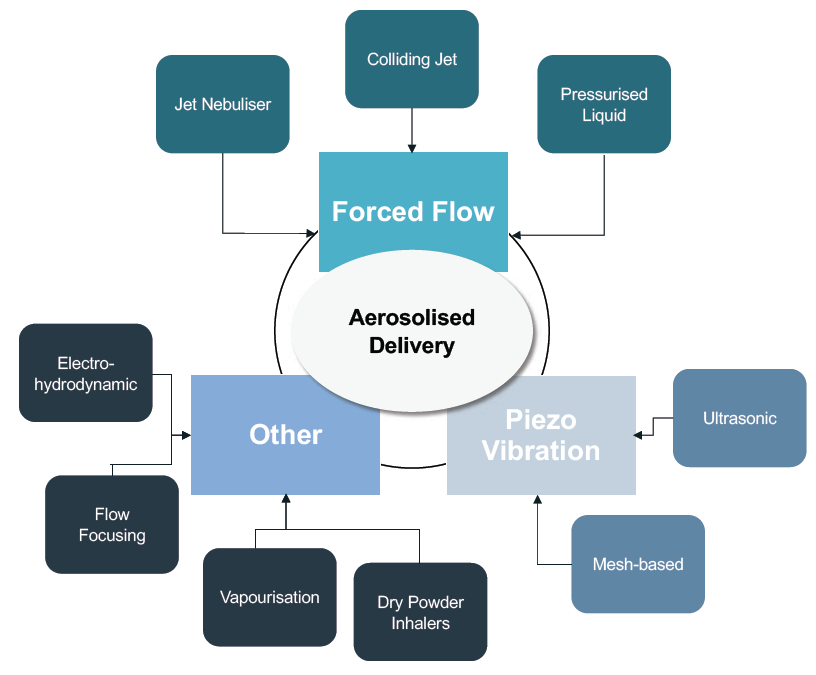
Figure 1: Different classes of aerosolised delivery.
“The technology decision is not as easy as assuming DPIs will remain more environmentally sustainable than pMDIs – DPIs may have the high ground currently, but newer propellants promise to level the score.”
The technology decision is not as easy as assuming DPIs will remain more environmentally sustainable than pMDIs – DPIs may have the high ground currently, but newer propellants promise to level the score once HFA152a and/or HFO 1234ze(E) are fully developed and launched – but they are not without issues.6 Furthermore, DPIs tend to use a number of high-value engineering polymers in their make-up and may not be as sustainable as some believe. A further complication (or opportunity?) comes from the increased use of soft mist inhalers (SMIs) (e.g. Boehringer Ingelheim, Merxin, Pharmaero (Hovedstaden, Denmark) and Well-Bridge (Suzhou, China)) which, while possible alternatives to pMDIs, are currently too expensive to compete on a cost basis, but that could change with the development of simpler atomisation mechanisms and increased reuse with simple refill cartridges.
“Packaging is also a key part of the environmental footprint.”
A propellant-free delivery approach may well lead to a lower overall global warming potential (GWP), but this is just one element of the overall design challenge. Creating a reusable device and reducing the environmental impact per dose is likely to deliver sustainability benefits but care must be taken to ensure that patient usability is not compromised. Furthermore, a key consideration will be the necessity of the chosen technology to deliver different, multiple drugs/combination therapies as well as different classes of drug. As inhalation continues to show potential as a delivery mode of choice for biologics, a device that has the potential to deliver both small molecules and biologics will be more attractive from a commercial and sustainability standpoint. Enabling device circularity (the principle that at the ultimate “end of life”, once the product can no longer be reused, it goes back into the supply chain, not landfill) together with creating a reusable platform suitable for delivering a wide range of therapies, maximises the useful life of the device and platform. Such an approach can improve the sustainability profile, compared with a single use, disposable design that is often limited to a smaller range of drugs (e.g. many monthly use DPIs). To a large extent, the issues with most common current devices are hard-wired based on the technology choices made when they were developed, in some cases, decades ago. For example, pMDIs must use a liquid propellent which increases their GWP. Alternative propellants have the potential to improve the situation, but not remove the issue completely, due to propellants being fundamental to the design principle.
DESIGN
Historically, we saw the move from traditional CFC-based propellants to HFAs driven by environmental pricing pressures, but now even these second-generation propellants are falling out of favour as they are also greenhouse gases.11 It is time to take the initiative and, while the suggestion to move away from pMDIs to DPIs may appear to make sense in the short term for some organisations (due to the impact of current propellants used), some patients cannot use DPIs and, furthermore, some medications do not exist in DPIs.6 Therefore, a move to DPIs cannot be the only short-term solution and is certainly not a long-term solution. Surely the long-term solution is to design the next universal platform for liquid inhaled drugs that can be adopted by the majority of pharmaceutical companies (just as the pMDI was for many years) – this is a challenge we are now equipped to meet.
For polymer-based consumer products, we are all aware of the drive to move away from single-use products and the need to change the “everything is disposable” mentality of modern consumerism. Is now the time to transition this ethos into drug delivery products; is it feasible? PA believes it is. Completely redesigning the inhaler provides the opportunity to create a paradigm shift in selecting inhaler component and packaging materials and manufacturing methods, which enables us to reduce the overall carbon footprint and target extending the product life (to reduce the carbon footprint/GWP per dose). For device components, moving to a more sustainable source of currently used plastics is a conservative step.
Alternatively, a bolder move is to consider changing to some of the “greener” forms of polymer, where alternative, lower-carbon feedstocks – such as 100% bio feedstocks – are used. Furthermore, by enabling patients to reuse the devices for longer periods and by ensuring circularity of use – by creating systems for the easy return of used devices for material recovery/recycling – more sustainable inhalers will emerge.
Often, the packaging side of sustainability in medical products is ignored; it has rarely been more than a basic necessity. However, many patients are now stimulated by initiatives in consumer packaging and will demand more from their medical products brands. In a holistic approach to sustainability, packaging is also a key element of the environmental footprint and must be considered in the sustainable redesign process. Learning from the consumer and consumer healthcare industries, and considering materials such as cellulose fibre-based polymers, which can be more sustainable than their petroleum-based cousins, may help further improve the sustainability profile.
“The growing environmental, societal and policy pressures to be more sustainable will become an inevitable hurdle for the inhaled drug delivery industry if we do not take the opportunity to transition and change now.”
All good product designs should consider the design of the supply and distribution chains. However, to develop more sustainable products, the circular elements of the supply chain should be considered and thus, how best to supply, reuse and recover materials in a truly circular way. Returning recovered materials to the original supply chain may make it possible to improve a product’s ultimate GWP. Unfortunately, this is not a given with drug delivery products due to the complex nature of the drug/device combination and the difficulties associated with separation and recovery of materials that could have drug still present. Thus, if we are ever to take on and address this problem, now is an ideal opportunity to consider the manufacture and recovery of materials in any new inhaler concept platforms – to build in QbD and SbD – considering the full environmental lifecycle and circularity. Frequently, manufacturing in wider product platforms has tended to favour specific geographies that provide the lowest cost offering for manufacture.
The supply chain, with more products containing thousands of parts, is complex and can involve increased environmental impact, increased GWP and increased carbon footprints for logistics/transport/supply chains. Furthermore, in many countries where the cost of production is low, the planetary cost of using carbon-intensive energy supplies, such as coal-fired power stations, is high and adds to the environmental cost of production. Thus, it is important that decisions based on sustainability and the environmental cost of production are considered, not just the financial manufacturing cost – the planetary cost of products has to be determined based on factual evidence and not unsupported dogma. An ill-considered approach can lead to low sustainability credentials due to large Scope 3 emissions,* leading to carbon-intensive product production.
As we progress through the next decade or so and consider alternative inhaler concepts, we may be able to consider a drive to be more local in the supply of raw material (where possible from circular recovery of used products and minimal virgin material). Inhalers are (after all) relatively simple, with typically less than 50 components compared with, for example, the thousands of components in a new car, and thus, the sustainability elements of inhaler and drug product manufacture may ultimately be driven by international and local legislation promoting or mandating local supply.12 Therefore, conceiving and building a device that enables at least partially decentralised supply chains where, as far as possible, products are manufactured and assembled locally/nearer to where they are used by patients, could lead to more sustainable inhalers. Of course, there are risks associated with technology transfer and particularly method transfer in drug manufacturing and supply, but do we really have to manufacture in only one or two locations and ship products all over the world? Furthermore, with the ongoing dynamic nature of the geopolitical landscape (e.g. current conflicts in Eastern Europe, price inflation for goods produced in China,13 etc.), a federalised model that does not rely on specific countries or sites for non-specialised manufacturing and assembly will lead to more secure supply and a potential for sustainable competitive advantage.
PLANETARY HEALTH
Planetary health requires the consideration of a number of elements to achieve the desired outcomes for the planet, in addition to those for the patient. Four of the key elements are circularity, impact, wider infrastructure and equity of access:
- By circularity, we mean consideration and understanding of the recyclability and reusability of the inhaler and the materials used in its manufacture, together with the aim of returning recovered material to the original supply chain.
- By impact, we consider other sources or entities that increase carbon footprint or global warming potential within the inhaler circular life, as a whole.
- By wider infrastructure, we consider the supply, utilisation and logistics involved in the delivery, recovery and ultimate disposal of the inhaler.
- By equity of access, we consider how easy it is for all patients to access and use any new solutions proposed; are there any limitations to who can use it, are materials globally available so it can be produced anywhere across the globe, will patients of all socio-economic backgrounds be able to obtain it and use it?
For example, in the bigger picture, there are downstream environmental impacts associated with poor adherence and avoidable hospital admissions. By creating better designs, improving usability, adherence and product access, there will be a sustainability benefit as well as a major patient benefit. Assessment of each of these elements in a more holistic manner is important in demonstrating the true sustainable nature of any new inhaler concepts. Only by following a more holistic approach will we ensure that future inhalers meet (and exceed) future environmental legislation.
This holistic assessment must be transparent and consider the complete end to- end process (E2E), from supply through distribution and recovery of the device and, in a similar way, the manufacture, supply and filling of the drug product. By more deeply understanding and assessing the overall lifecycle process in terms of circularity, cost and carbon, planned changes or new concepts for a product can be quantified in terms of increasingly demanding sustainability requirements and a sustainable business case can be delivered. Such an approach that looks at E2E processes is likely to show that, from a sustainability perspective, current DPIs and SMIs may be better than current pMDIs; but they are not (in their present form) a sustainability silver bullet when considering the whole lifecycle of the inhaler.14
Furthermore, by considering and quantifying the wider benefits to patients and healthcare providers of a new design (whether that be increased access, improved adherence, etc.), we can demonstrate the broader healthcare system-wide impacts and value. Overall, this final assessment step in creating a new generation of inhaler will be a crucial step for the future. As regulators, specifiers and users begin to differentiate between devices using their overall carbon footprint and sustainability credentials, new technology and new designs will achieve little if the sustainability credentials cannot be demonstrated.
In summary, the growing environmental, societal and policy pressures to be more sustainable will become an inevitable hurdle for the inhaled drug delivery industry if we do not take the opportunity to transition and change now. While the figures for the global environmental impact of inhalers may be low, for individual companies and healthcare providers, they can be significant, and it is suggested that we both need and can deliver new inhaler concepts to make them better for patients, the planet and sustainable by design.
By focusing on the technology used, performance required, the design of materials, the inhaler and its supply chain, and by close consideration of the user and planetary needs – demonstrating sustainable credentials – we have the opportunity to deliver a paradigm shift. If we take these factors into account and see them as an opportunity to release ingenuity and help patients become more engaged with their devices, we can ensure inhalers have a long, sustainable future ahead.
PA believes that, as pharma companies transition from drug suppliers to partners caring for patients, there will be parallels to trends in consumer markets, increasing the importance of sustainability in brand reputation and patient retention. Convincing key pharma decision makers and global healthcare providers that customer choice is increasing is a challenge, but the shift is happening.
*(Emissions that are the result of activities from assets not owned or controlled by the reporting organisation, but that the organisation indirectly impacts in its value chain.)
REFERENCES
- “Sustainable inhaler prescribing incentive announced”. MIMS online, Aug 27, 2012.
- “NICE encourages use of greener asthma inhalers”, NICE, Apr 8, 2019.
- “Consultation on the future regulation of medical devices in the United Kingdom”. Gov.uk, Sep 16, 2021.
- “Sustainable Medicines Partnership”. YewMaker, Accessed Oct 2022.
- “About Montreal Protocol”. Unep.org, Accessed Oct 2022.
- Pritchard JN, “The Climate is Changing for Metered-Dose Inhalers and Action is Needed”. Drug Des Devel Ther, 2020, Vol 14, pp 3043–3055.
- O’Rourke K, “Six Pharmaceutical Firms Taking a Lead in Sustainability”. CSRWire, Mar 20, 2020.
- Seeney P, “The Options for Creating a More Sustainable Inhaler”. ONdrugDelivery, Issue 106 (Apr 2020), pp 22–25.
- “Environmental effect of Inhalers Crib Sheet for health care Professionals”. NHS, Jul 1, 2021.
- Robinson J, “NHS England has no plans for a national inhaler recycling scheme despite net zero ambitions”. The Pharmaceutical Journal, Aug 19, 2021.
- DeWeerdt S, “The environmental concerns driving another inhaler makeover”. Nature.com, May 13, 2020.
- “The Biden-Harris Plan to Revitalize American Manufacturing and Secure Critical Supply Chains in 2022”. The White House, Feb 24, 2022.
- “Double-Digit Price Hikes on China Exports Add to Inflation Risk”, Bloomberg, Oct 19, 2021.
- Robinson J, “Greener inhalers: are we setting the wrong targets?”. Pharm J, Oct 28, 2021.

