Citation: Philpott C, Hawley M, French N, “Meaning-Centred Product Development: the Key to Successful Connected Disease Management”. ONdrugDelivery, Issue 121 (Jun 2021), pp 20–24.
Christina Philpott, Miles Hawley and Natasha French, discuss the future of connected disease management and the potential benefits for asthma treatment.
Asthma affects over 300 million people worldwide.1 As a lifelong condition with no cure, implementing an effective management strategy that combines patient education and prescribed medication is currently recommended as the most successful way to treat asthma in adults by charities such as Asthma UK.2
“Developing connected respiratory disease treatments is far from simple, requiring collaboration between complex networks of parties with differing expertise and interests, with years – sometimes decades – of development before launch.”
Whilst paper-based tools and regular GP and asthma nurse appointments are established aspects of monitoring and controlling asthma, advances in technology have provided a much greater opportunity to obtain insights into patients’ device usage, compliance and lived experience of asthma. These insights can be used to enable better treatment outcomes, whether informing patient-facing interfaces, providing additional information to healthcare professionals (HCPs) or feeding back to medical device developers and component manufacturers – shaping and improving future product pipelines and new condition management approaches.
Outside of medicine, the growth and omnipresence of Internet of Things (IoT)- and AI-enabled technologies are driving targeted and personalised solutions in analogous categories – directly influencing what patients are coming to expect from their healthcare solutions.
Connected fitness wearables such as FitBit and Garmin watches have brought biometric monitoring into everyday life. Menstruation-tracking apps have made symptom prediction tangible and personalised. The covid-19 pandemic has accelerated people’s fluency with virtual interaction and their acceptance of self-testing, making telemedicine and remote healthcare more achievable and accessible than ever.
The developments in these analogous categories are shaping not just how patients expect their medical devices to look, feel and perform but how they expect information to be communicated and what they define as successful condition management for themselves as individuals. For instance, an arbitrary assessment of “improved symptoms” will no longer be satisfactory when patients are accustomed to consumer offerings that measure biomarkers to the percentile improvement.
Developing connected respiratory disease treatments is far from simple, requiring collaboration between complex networks of parties with differing expertise and interests,3 with years – sometimes decades – of development before launch. The technologies that can enable advanced, connected asthma solutions already exist. However, the variety of specialist expertise and technical capability required to successfully apply these technologies to the treatment of pulmonary disease is currently held by many disparate parties. Experts in all aspects of pulmonary disease management and connected data technologies must work together collaboratively to drive continuous improvement towards the common goal of safer and more effective treatments.4
It is therefore essential that connected health platforms are developed with foresight as a priority – an ability to understand how emerging technological developments and legislation changes can translate into successful product offerings by the time of launch. Critical to ensuring this is establishing direct ties with patients3 and identifying the strategic opportunities that provide commercial differentiation alongside meaningful patient benefits.
Meaning Centred Design is a research-led approach to brand and product development pioneered by Recipe Design, a strategic design consultancy based in London. The team at Recipe has spent over a decade practising Meaning Centred Design to help clients achieve growth through product and service innovation across the healthcare and home sectors.
“ADD•FLO proposes a new dynamic for asthma management that bridges prescription medication with evolving attitudes in healthcare, wellness and connected devices.”
THE MEANING CENTRED DESIGN APPROACH
Meaning Centred Design uses a range of techniques such as semiotic and discursive analysis, expert and stakeholder interviews, iterative co-design sessions with patients and HCPs, and technology forecasting. Insights drive strategic responses that can be used to inform product pipelines that factor in social, economic and technological developments. Understanding how meanings are likely to shift is a powerful way of identifying design opportunities that intersect, blend and define changing attributes to develop offerings that resonate deeply with people.
EVOLVING THE MEANING OF ASTHMA MANAGEMENT
When examining the potential for connected asthma management platforms, there are many evolving meanings running in parallel, with the opportunity to intersect in new and differentiated ways. To articulate these shifts in meaning, Recipe Design has developed ADD•FLO, a conceptual study that explores a holistic, future-facing platform approach to asthma management, grounded in insights obtained from over 15 years of user research and product development with partners in the respiratory health and metered dose inhaler (MDI) industries.
ADD•FLO uses a unique combination of digital and physical tools (Figure 1) that enable asthma patients to better understand and manage their condition at home. Informed by the shifts in meanings spanning multiple categories of products, ADD•FLO proposes a new dynamic for asthma management that bridges prescription medication with evolving attitudes in healthcare, wellness and connected devices.

Figure 1: ADD•FLO combines a smart hub, an MDI actuator and a connected app.
“With an increased understanding of the analogous factors that can cause, affect and exacerbate asthma… connected healthcare platforms can help to explore the impact of behavioural changes and alternative treatments that are reported to alleviate asthma symptoms.”
ANTICIPATING EVOLVING PATIENT EXPECTATIONS AND NEEDS
Many patients rarely, or reluctantly, describe themselves as “sufferers” – or, indeed, “patients” – in an effort not to self-identify as sick or vulnerable. They choose to manage their condition as discreetly as possible, rejecting overly medicalised inhalers and shunning any connotations of ill-health.
There are also anecdotes of patients who have requested a more stylised inhaler, citing the MDI used by Le Chiffre in the film Casino Royale as something desirable and aspirational. Similarly, Recipe’s award-winning work on the Mundipharma (Cambridge, UK) K-Haler not only provided improved device compliance and competitor differentiation but led to the youngest and least compliant patients describing the inhaler as “cool” – a product they were happy to be seen with, resulting in increased engagement with condition management.

Figure 2: The ADD•FLO smart hub displays notifications and provides UV sterilisation.
In response to these shifts, the ADD•FLO study explores a design language that combines the trusted reassurance of medical devices with premium forms, materials and finishes. A smart hub base (Figure 2) creates a designated place for asthma care in the home, displays notifications generated in the ADD•FLO app and provides UV LED sterilisation for the MDI actuator and spirometry mouthpiece to ensure it stays clean and hygienic between uses.
Patients are also encouraged to perform breathing exercises through the actuator before administering their daily preventer medication. There is increasing evidence that practising breathing exercises can improve inhalation technique5 and reduce reliance on rescue medication,6,7 with the potential for further positive implications on both mental health and general health, such as lowering blood pressure.8
These factors combine to create a system of products that sit comfortably and proudly in the evolving smart home environment, accommodating increased awareness of hygiene in a post-covid-19 world and responding to evolving patient attitudes about blended mental and physical health interventions.
USING STRATEGIC COMBINATIONS OF EXISTING TECHNOLOGIES
With an increased understanding of the analogous factors that can cause, affect and exacerbate asthma1 – such as indoor and outdoor air quality, airway microbiome and dietary factors – connected healthcare platforms can help to explore the impact of behavioural changes and alternative treatments that are reported to alleviate asthma symptoms, such as practising breathing exercises and consuming certain vitamins.9 The ADD•FLO app looks to further this understanding – on both an individual patient level and from a global health perspective – with the potential to contribute data to clinical studies or directly inform and improve new product development.
Patients can manually track their symptoms alongside data imported from third-party apps, such as biometric data from wearables, diet, location and weather information (Figure 3). Over time, machine-learning capabilities can provide rich insights about the factors that may be exacerbating the patient’s symptoms, finding correlations it would otherwise be difficult to observe and prompting the patient to intervene to avoid preventable suffering.
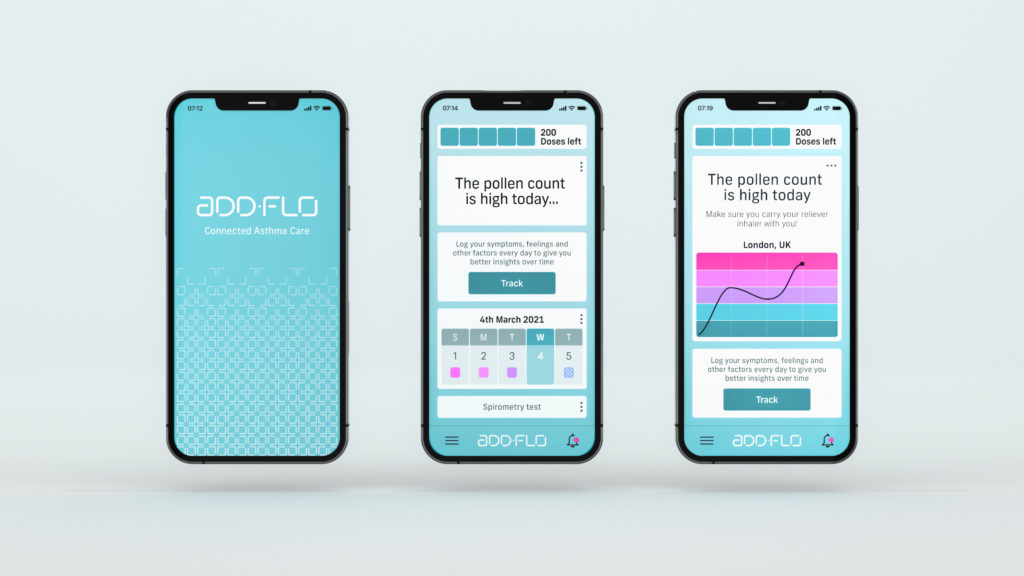
Figure 3: The app provides insights from aggregated data.
“By prioritising the patient’s experience of the platform – ensuring ease of use, providing meaningful insights and reminders, establishing habitual behaviours and supporting compliance – patients can access marked improvements and benefits that help them to feel more informed and more in control.”
Additionally, the ADD•FLO smart hub automatically logs each actuator use to inform an activity log and dose-counting function on the app, estimating how much medication is left and reminding patients to renew prescriptions, as required. In theory, this could prevent the need for add-on mechanical or electronic dose counters by using digital platforms and predictive analytics to estimate the contents remaining in a drug cannister.
By prioritising the patient’s experience of the platform – ensuring ease of use, providing meaningful insights and reminders, establishing habitual behaviours and supporting compliance – patients can access marked improvements and benefits that help them to feel more informed and more in control.
ESTABLISHING AGILE SYSTEMS THAT RESPOND TO FUTURE DEVELOPMENTS

Figure 4: An additional mouthpiece enables patients to perform spirometry tests at home.
In line with evolving sustainability legislation, the ADD•FLO actuator houses an MDI cannister of liquid medication, which can be replaced when depleted by unscrewing the top section of the actuator. The actuator can then be reused, kept sterile by the smart hub, reducing both the need for disposable actuators and the overall packaging necessary to fulfil renewed prescriptions. This modular, sustainable approach to actuator design can be applied to future MDI solutions, especially as new propellants and canisters are introduced in line with changing sustainability legislation.
The ADD•FLO system also incorporates an additional mouthpiece (Figure 4) which enables a spirometry test to be performed by the patient at home. Test results can then be shared with their HCP remotely via the app, overlaid with the data obtained from tracked symptoms, to provide insight into the effectiveness of their current prescribed treatment and guide the HCP on the necessity for medical interventions.
Remote clinical assessments conducted by the patient, in their own home, have the potential to reduce the need for in-person appointments, as well as reducing footfall in clinical settings – a trend that may continue to be advantageous beyond the covid-19 pandemic. This approach empowers the HCP-patient relationship, driving appointment efficiency, whilst offering patients more autonomy and control.
Laying considered foundations for developments in legislation and anticipating the disruption of global shifts, such as those brought about by the covid-19 pandemic, can enable device developers and manufacturers to remain agile and responsive to change, rather than reactive.
THE EVOLVING FUTURE OF CONNECTED ASTHMA MANAGEMENT
To ensure new connected healthcare platforms are successful, multiple factors must be considered in parallel. As well as the patient and HCP experience, other stakeholders must be considered, taking into account emerging drug delivery technologies, manufacturing methods, sustainability targets and data privacy legislation that will continue to shape and govern the connected healthcare category.
ADD•FLO articulates a potential future of connected condition management. It explores how asthma treatment could evolve, drawing on insights from parallel and analogous categories such as wellness products and smart home technology. It proposes a solution that sits at the point where the meanings of these categories will intersect in the near future, with considerations to the manufacturing and regulatory constraints surrounding the category as they emerge and evolve simultaneously.
ADD•FLO demonstrates the effectiveness of a Meaning Centred Design approach; the concept offers a holistic and future-facing perspective for connected health that unifies the many ideas circulating in the category, whilst addressing many long-standing issues.
REFERENCES
- “The Global Impact of Respiratory Disease – Second Edition”. Forum of International Respiratory Societies, May 2017.
- “Managing asthma in adults”. Asthma UK, 2019.
- Jung B, “The Future of Connected Asthma and COPD Care: a Network Perspective”. ONdrugDelivery Magazine, Issue 98 (Jun 2019), pp 18–22.
- Burnett H, “How Emotional Intelligence is Driving Improvements and Meeting the Challenges in Pulmonary Drug Delivery”. ONdrugDelivery, Issue 114 (Nov 2020), pp 33–36.
- Murphy A, “How to help patients optimise their inhaler technique”. Pharmaceutical, 2016, Vol 297(7891), Article 20201442.
- Thomas M, Bruton A, “Breathing exercises for asthma”. Breathe, 2014, Vol 10, pp312–322.
- “Complementary therapies and asthma”. Asthma UK, 2019.
- Elliott W, Izzo J, “Device-guided breathing to lower blood pressure: case report and clinical overview.” MedGenMed, 2006, Vol 8(3), p 23.
- Menon B et al, “Evaluation of vitamin D in bronchial asthma and the effect of vitamin D supplementation on asthma severity and control: A randomised control trial”. Breathe, 2014, Vol 44, p 4049.

