Citation: Reynolds J, “Training Devices and Patient Education Play a Crucial Role in the Self-Injection Drug Delivery Market”. ONdrugDelivery, Issue 113 (Oct 2020), pp 30–34.
BIOPHARMACEUTICALS: AN INDUSTRY MARKED BY GROWTH AND INNOVATION
“The rising number of parenteral medications has prompted drug and packaging manufacturers to continue seeking more sophisticated delivery systems. By 2017, there were over 100 injectable drug products available in prefilled syringes and an ever rising number of pipeline drugs targeted for delivery by this method.”
The biopharmaceutical industry has experienced incredible exponential growth in recent decades. Annual revenues have increased from US$4.4 billion (£3.4 billion) in 1990 to $275 billion (£213 billion) in 2018 (a 6,250% increase) and now represent more than 25% of the total pharmaceutical market.1
A primary driver of this rapid expansion is the pioneering pursuit of biologics to treat the growing rate of chronic diseases.2 Other factors fuelling the industry’s robust economic growth are technological advancements, such as the use of smart data, machine learning and wireless connectivity, and the ongoing progress towards developing new products and services to better meet patients’ needs and the challenges they confront in the daily use of their prescribed therapeutics.3
The Evolution of Injection Devices and Prefilled Syringes
Injectable drug delivery systems have come a long way from conventional syringes packaged with simple vials to include prefilled syringes, autoinjectors, pen injectors and needle-free systems. The origin of prefilled syringes dates back to the 1950s when they were introduced in a polio vaccination campaign.4
The rising number of parenteral medications has prompted drug and packaging manufacturers to continue seeking more sophisticated delivery systems. By 2017, there were over 100 injectable drug products available in prefilled syringes and an ever-rising number of pipeline drugs targeted for delivery by this method.5
OPPORTUNITIES AND CHALLENGES FOR SELF-INJECTION DRUG DEVICES

Figure 1: For patients who lack hands-on access to an HCP, robust patient training and proper onboarding can further support them during this uptick in telemedicine appointments.
The expanding development of biologic drugs to address chronic diseases, from diabetes and multiple sclerosis to Crohn’s disease and rheumatoid arthritis, has resulted in an increasing cohort of patients who rely on self-injection devices to administer their medications at home. Supporting this trend are advances in the design of patient-centric devices, driven by usability and intuitiveness, which are transforming biologic drug delivery.6 The involvement of training devices and patient education could be essential to the success of this transformation.
But with opportunity comes challenges; nearly half of health care professionals (HCPs) who prescribe self-injecting drug delivery devices do not train patients on how to self-inject correctly.6*
The covid-19 pandemic has helped to bring telemedicine into the mainstream as a safe and convenient alternative to traditional in-person medical care. Nearly 60% of respondents to a survey conducted in mid-March 2020 indicated that covid-19 made them more likely to consider using telehealth services in the future, yet over 40% expressed concerns about the ability to be properly diagnosed or treated in a virtual setting.7 For those patients who lack hands-on access to an HCP, robust patient training and proper onboarding can further support them in adhering to their therapeutic treatments (Figure 1).
The Benefits of Training Devices Combined with Patient Education
“The covid-19 pandemic has helped to bring telemedicine into the mainstream as a safe and convenient alternative to traditional in person medical care.”
Noble, an Aptar Pharma company, first saw the need for better self-injection training at the beginning of the 2010s. Since then, it has become a global leader in the development and delivery of medical device training solutions, patient onboarding strategies and multisensory products for patients and HCPs that aim to improve patient adherence and, ultimately, healthy outcomes.
And yet, the need for ongoing patient training persists. While biologic and drug delivery advancements are giving more patients with chronic conditions greater access to therapeutic medications, some patients are non-adherent due to lack of training, improper use and recall erosion
- 49% of HCPs do not train patients to correctly use their self-injection devices.6*
- 84% of patients do not use an autoinjector correctly.8**
- 90% of treatment information is forgotten in a week if patients do not practice at home, a phenomenon attributable to the “forgetting curve” theory that, without practice and repetition, retention and recall degrade over time.9
An Empirical Look at Patient Training
In 2018, Noble conducted a survey to understand better how patients learn, retain and recall information. This longitudinal study explored whether the use of injection training devices and other stimuli to help reinforce memory could, over a period of time, lead to decreased memory decay, fewer device errors and improvements in the onboarding experience for patients who self-inject.
To begin the study, participants across three cohorts – nine participants per cohort – attended an introductory session where they received self-injection training, just as they would in a doctor’s office if they were prescribed a self-injection course of therapy.
During this first session, researchers replicated an optimal introductory in-office learning experience between an HCP and a patient. This session focused on introducing participants to the drug delivery device and then training them on how to use it with a demonstration device that did not include medication or a needle.
Afterwards, participants could practice on themselves with a training device, with researchers present. Participants were also given feedback and recommendations for improvement, as would occur during training with an HCP. After the 45-minute training session, they were sent home.
To understand the effects of having access to a training device in-office only, cohort A – the control group – was sent home with only the instructions for use (IFU). This cohort was not intended to represent the minimum amount of training a patient may receive, but to set a baseline for evaluating the effects of having additional support, such as training materials, at home. Cohort B was sent home with both an IFU and a training device that mimicked the actual device they would self-inject with later in the study, and Cohort C was given both the IFU and the training device, as well as an interactive training video to use at home.
Participants were instructed to practise at home as little or as often as they preferred and were told to keep track of how many times they used their materials. Participants then did not hear from researchers for 14 days, allowing them to practise with the various materials as frequently or infrequently as they preferred. The purpose of this was to uncover the correlation between successful and unsuccessful self-injections and the participants’ access to training materials.
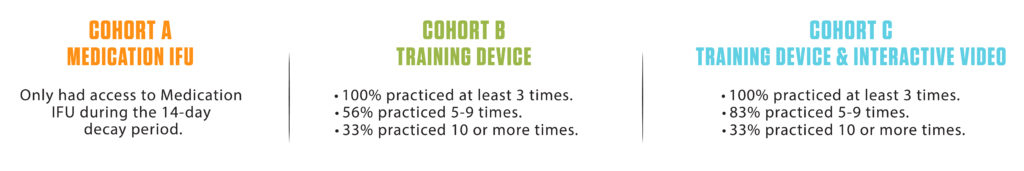
Figure 2: Research found participants with additional training resources were more engaged during the decay period.
The study confirmed that when patients are provided with materials to practise with at home, engagement in their therapy increases (Figure 2).
- 100% of participants practiced at least three times
- 70% of participants with demonstration devices (cohorts B and C), on average, practiced five-to-nine times
- 33% of subjects practiced 10 times or more
- 92% of participants indicated they prefer to receive a training device to take home and practice (Figure 3).

Figure 3: The majority of participants stated how important a training device would be to have in the home for practice.
Moreover, the study concluded that 100% of cohorts B and C completed all critical steps for a successful self-injection, while only 44% did so from cohort A.
Noble’s Training Solutions Aim to Address the Needs of Today’s Patients
Human behaviour and user experience are critical elements of a patient-centric training solution. Noble’s training devices – including autoinjectors, prefilled syringes, on-body and respiratory devices – are calculated to mimic the feel, force and function of the actual drug delivery device so that patients can practise at home; potentially resulting in less error and increased device familiarity.
“Noble’s training devices – including autoinjectors,
prefilled syringes, on-body and respiratory devices –
are calculated to mimic the feel, force and function
of the actual drug delivery device so that patients can practise at home; potentially resulting in less error and increased device familiarity.”
Noble also provides IFU for its training devices to help guide patients through proper administration prior to using the true drug delivery device. Specifically designed to complement the actual device, the training IFUs address human factors such as literacy-level messaging, multiple language options and simple step-by-step instructions.
Partnering with Biopharma to Advance Healthy Outcomes
To achieve the goal of fostering healthy outcomes for patients who self-administer their drug therapies, Noble partners with leading biopharmaceutical companies and original equipment manufacturers (OEMs) to develop and launch innovative training platforms and holistic solutions.
One such partnership is with BD. Noble’s robust programme for the BD UltraSafe™ passive needle guard portfolio involves designing and manufacturing demonstration and onboarding devices, as well as supporting materials, with the aim of strengthening pharma’s commercial launches and improving patient adherence.
The newest addition to Noble’s line of demonstrators for the BD UltraSafe™ needle guard portfolio is the BD UltraSafe Plus™ 2.25 mL. Proprietary features of Noble demonstration devices include a resettable locking needle guard that simulates the safety systems with the ability to reset the device for multiple training sessions, and an encased faux needle designed to simulate the forces and feel of an injection.
From clinical trials through to post-launch, Noble’s integrated approach includes human factors studies and patient experience mapping; launch strategy and pre-launch training summits; training device distribution and fulfilment; and patient and HCP engagement programmes. This combined comprehensive approach benefits not only the patient, but also Noble’s partners, with improved speed to market, lower cost of entry and the ability to customise training devices to brand specifications.
CONCLUSION
Biopharma manufacturing is expected to continue evolving and adopting new and improved technologies, contributing to a global biotechnology market that is expected to surpass $775 billion (£601 billion) by 2024.1 When it comes to the rising number of self-injection therapies, Noble recommends that patient training and education be part of the standard of care for biopharmaceutical companies and OEMs to help build more confident, healthy – and ultimately, adherent – patients who self-administer.
REFERENCES
- Rader R, Langer E, “Biopharma Market: An Inside Look”. Pharma Manufacturing, November 15, 2018.
- “Biotechnology Market will expand at 9.9% CAGR to hit $775 Billion by 2024”. Press Release, Global Market Insights, January 23, 2019.
- Event Web Page, “PDA Universe of Pre-Filled Syringes & Injection Devices Conference 2019”. Accessed 2019.
- Company Web Page, Becton Dickinson, October 2020.
- “Prefilled Syringes Market (4th Edition), 2016–2026”. Press Release, ReportBuyer, April 5, 2017.
- Lang V, Nalan D, “Combination Product Patient Training: How are Patients Trained and Who Conducts the Training?”. Am Soc Mech Eng, Frontiers in Biomedical Devices, 2018 Design of Medical Devices Conference.
- “Survey Report: Americans’ Perceptions of Telehealth in the Era of COVID-19”. Sykes. March 2020.
- Potera C, “Misuse of Autoinjectors And Inhalers”. Am J Nurs, 201, Vol 115(3), p17.
- Kohn A, “Brain Science: The Forgetting Curve – the Dirty Secret of Corporate Training”. Learning Solutions, March 13, 2014.

