To Issue 131
Citation: Udale R, Jameson H, “Waiting with Bated Breath – What’s in Store for 2022”. ONdrugDelivery, Issue 131 (Apr 2022), pp 6–9.
Rob Udale and Heather Jameson discuss the exciting developments taking place in the design of inhalation devices and share their predictions for the top five inhalation trends to watch as 2022 unfolds, and beyond.
SUSTAINABILITY AND GREENER LIFECYCLE MANAGEMENT
“In addition to reducing the carbon footprint of individual inhalation devices, medical device companies are also increasingly committed to finding carbon-neutral manufacturing solutions and assessing the impact of their devices’ full lifecycles.”
November 2021 saw the largest climate change conference of its type to date, COP26, bringing a new wave of eco-awareness that has permeated almost every industry. Medical engineering is no exception, and we are seeing early signs of a revolution in the sustainability and reusability of inhalation devices.
Over the last half-century, many drug delivery devices have been designed with disposability in mind. Disposability has its advantages:
- High-volume manufacture brings efficiencies of scale
- Single-use, disposable devices can have fewer use steps and can be easier to use
- It can be easier to guarantee user safety with a disposable device.
But if we look back to some of the first inhalation devices from the late 20th century, such as Boehringer Ingelheim’s Aerohaler or GlaxoSmithKline’s Diskhaler, we find a very different story. Those early devices were reusable with a loadable primary pack.

Figure 1: The new reusable version of Boehringer Ingelheim’s Respimat® has a 71% smaller carbon footprint after six months of use compared with its disposable counterpart.
Now, in 2022, we are beginning to see a move “back to the future” and a return to those reusable devices (Figure 1). The driving forces for this move include:
- Patients and other stakeholders becoming more sensitive to the environmental impact of fully disposable devices, in particular that from plastic waste.
- The current generation of devices tending to be more complicated and costly than the previous generation. For example, pressurised metered dose inhalers (pMDIs) are now more likely to have a dose counter or a breath actuation mechanism. The economics of fully disposable devices sets an upper limit on their cost.
- The “connectivity” aspect of many new devices. The electronics and batteries that are typically involved lend themselves to reusable modules.
- Potential future changes in reimbursement structures to incentivise reuse.
In addition to reducing the carbon footprint of individual inhalation devices, medical device companies are also increasingly committed to finding carbon-neutral manufacturing solutions and assessing the impact of their devices’ full lifecycles. It was fantastic to hear announcements at COP26 that FTSE100 companies, including AstraZeneca and GSK, are now committed to eliminating their contribution to climate change by 2050.1
This reinforces messaging earlier in 2021 when both AstraZeneca and Chiesi announced a commitment to develop pMDIs with near-zero global warming potential.2,3 One way that manufacturers are planning to achieve this is by recapturing some of the embodied energy within the waste materials; Chiesi launched an inhaler recycling scheme in February 2021 that covers any inhaler from any manufacturer, which could reduce the waste caused by the 73 million inhalers prescribed each year in the UK4 – change is afoot!
Highlighting this industry trend, springboard has been working on several projects that aim to reduce the environmental impact of inhalation devices, frequently following methods defined in the ISO 14000 standard on environmental management. In line with this, lifecycle assessments should be undertaken and updated throughout the device development process to ensure that devices meet the requirements of both the end-user and wider stakeholders. We should expect to see more devices that:
- Are either reusable or have reusable subassemblies.
- Have reduced embodied energy due to the smart use of biopolymers and recycled plastics or the selection of materials and manufacturing methods that have reduced environmental impacts.
- Are designed with device end-of-life in mind, including active management of their waste streams – recover, reclaim and reuse are core imperatives here.
This is a trend that we very much hope to see continued in 2022.
SOFT MIST INHALERS
With Spiriva, a successful drug for the treatment of chronic obstructive pulmonary disease (COPD), beginning to come off-patent across the globe, several companies have designs for generic alternatives in the pipeline, from Merxin to Softhale (Diepenbeek, Belgium), and we should expect other novel soft mist device platforms to follow (Figure 2). These companies will be looking to capitalise on the established properties that make soft mist designs so attractive, such as:
- Their aerosolised and propellant-free drug solutions are expelled in a slow jet, which reduces undesired oropharyngeal deposition.
- This slower jet velocity makes it much easier to perform the sequence successfully between actuation and inhalation.
- The aerosol fine droplet fraction from Respimat, a very successful soft mist inhaler, is reported to be approximately double that of a pMDI, meaning half the dose with a Respimat can achieve the same therapeutic outcome as the full dose administered by a pMDI.5
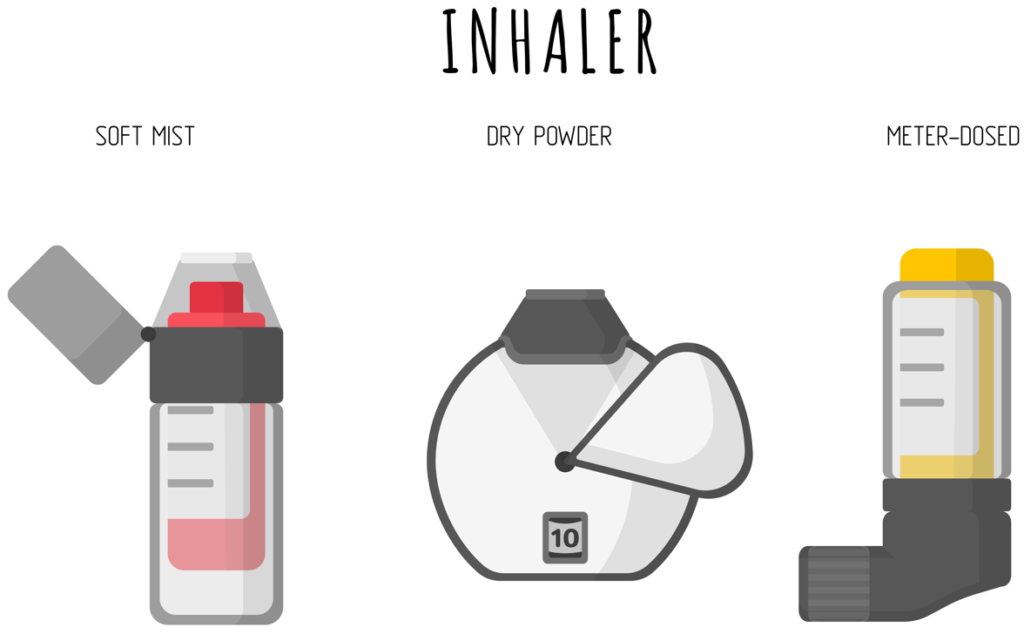
Figure 2: Soft mist inhalers are likely to become a staple of the inhalation market alongside DPIs and pMDIs.
We could expect to see soft mist inhaler designs with new developments to the drug storage container that allow them to contain more doses and potentially to deliver ethanol-based formulations, such as corticosteroids. It is likely that new designs will also seek to minimise the need for overfilling, thereby reducing costs, especially for higher value drugs such as biologics – the third trend.
“Over the last decade, there has been a socio-medical trend towards reduced dosing frequency to minimise intrusion of therapies into patients’ lives.”
BIOLOGICS AND LARGER DOSES
Biologics for inhalation is another area to watch for in 2022 – continued growth and recent advancements in biologics and biosimilars6 across industries (including parenteral drug delivery) are likely to filter through to the design and development of inhaled drugs and their delivery devices. An example of this is seen in the continued interest in technologies that offer non-parenteral insulin delivery solutions.
Additionally, over the last decade, there has been a socio-medical trend towards reduced dosing frequency to minimise intrusion of therapies into patients’ lives. In recent years, a focus on delivering larger dose volumes has gone some way towards addressing this unmet need. Of course, solutions with reduced dosing frequency require a correspondingly greater focus on patient adherence, including technology that assists users through reminders and data tracking. Therefore, alongside the drive towards these larger doses, we will continue to see the trend towards smart inhalation devices.
Inhalation may become the delivery method of choice to address these advancements in 2022 and beyond. Of the inhalation platforms, dry powder inhalers (DPIs) and nasal delivery systems are well suited to large-molecule delivery, so expect exciting growth in this area.
“Smart devices have been heralded as a major trend for the future for at least the last decade, and many will be wondering whether 2022 will be the year that finally brings their widespread adoption.”
CONNECTED HEALTH
Smart devices have been heralded as a major trend for the future for at least the last decade, and many will be wondering whether 2022 will be the year that finally brings their widespread adoption. Generally, the old adage holds true: “In the field of medical technology, evolution rather than revolution often wins out.”
The drive towards reusable devices and the increased interest in delivering larger molecules with reduced dosing frequency may be the impetus needed finally to help establish smart inhalation devices. This progress will be incremental, as there are still significant challenges within device design:
- How to demonstrate value to the payer.
- How to tackle the issue of data collection and patient trust when very few consumers believe companies handle their data responsibly.7
- How to manage the device strategy – as a connected add-on or upgrade, or as a fully integrated device from the ground up.
- How to mitigate cybersecurity risks and navigate a regulatory landscape that is currently struggling to keep up with the rapid pace of development.
However, there are encouraging signs that these hurdles are being overcome. An example of this is Teva’s CareTRx inhaler sensor, which is already being tested in the UK NHS.8 Medical device manufacturers are realising the need for high-quality input data, gathered in a way that does not burden the end-user. Devices and their apps need to fit into patients’ lifestyles, match their needs and have a prosumer experience in line with the world of consumer electronics.
Additionally, we may see a greater focus on device training incorporated within the user experience to tackle the issues of incorrect technique on the user’s part, either external to device usage, such as through a connected app, or as an integrated feature.

Figure 3: Nasal drug delivery is set to be an area with huge potential for growth.
NASAL INHALATION
The final trend to watch for in 2022 is nasal inhalation, a delivery method with huge growth potential (Figure 3). The market was valued at US$7.8 billion (£5.7 billion) in 2018 and is predicted to reach close to $12 billion by the end of 2025.9 Nasal inhalation systems offer several attractive benefits:
- A less-invasive drug delivery method that is preferable to injections. Factors include ease of learning and use, device portability, safety and comfort.10
- Ability to deliver drugs across the blood-brain barrier.
- Faster absorption than is possible with enteral solutions.
- Better molecule survival rates than oral delivery forms.
- Best inhalation delivery method for larger molecule solutions, including biologics.
There is active research towards developing drugs that can bypass the blood-brain barrier to aid in treating conditions such as schizophrenia and epilepsy. Nasal inhalation offers a powerful solution; consequently, there has been recent interest in harnessing this delivery system to provide enhanced delivery of established molecules, such as ketamine and cannabinoids, which will likely have a faster route to market than novel chemicals.
“Nasal drug delivery is a highly versatile method of administration for both local and systemic drugs, for emergency doses and managing long-term conditions, and in preventative vaccines.”
One particularly pertinent use of nasal inhalation systems is that of vaccine delivery. Covid-19 has led to significant investment in the global vaccines market, and this can be expected to continue as co-operative international efforts to vaccinate developing countries get underway. Nasal inhalation of vaccines has several key advantages – needle-phobia affects 3.5%–10% of the UK population11 and may drive vaccine hesitancy, and nasal vaccines are able to instigate mucosal immunity directly at the site of infection.12 Another important benefit lies within the “rescue treatment” setting. Numerous medical conditions call for swift drug administration and rapid onset. Using a nasal spray that provides a rapid onset is an ideal solution that can be used by anyone; examples can already be seen in emergency-use medications, such as naloxone for opioid overdose.
Finally, advancements in nasal inhalation have exciting implications for biologics research. Successful nasal delivery of peptides has already been demonstrated for the treatment of conditions such as osteoporosis, haemophilia and vitamin B12 deficiency. However, larger molecules continue to present a challenge to nasal inhalation methods due to the limited permeability of the nasal mucosa, and further research will be required to develop a solution.
Nasal drug delivery is a highly versatile method of administration for both local and systemic drugs, for emergency doses and managing long-term conditions, and in preventative vaccines. Key to this is the flexibility of the device to the drug’s formulation (its suitability for water-based or hydroalcoholic formulations, suspensions, emulsions and powders) and the fact that the nasal devices tend to be convenient, discreet, easy to use and easy to carry.
To some degree, nasal inhalation does lag behind other inhalation devices in the incorporation of dose counters, locks and connected elements. We may therefore see more nasal delivery devices with these features incorporated in the future.
FINAL REMARKS
This article has outlined five key inhalation trends to watch in 2022. Some perennial themes emerge – connectivity, efficacy, safety, cost-efficiency and ease of use. There are also, however, themes that are products of the rapid changes the world has undergone over the last few years; primarily a renewed interest in alternative vaccine delivery methods and a commitment to sustainability and greener products that are hopefully here to stay.
REFERENCES
- “COP26 Sees UK Businesses Lead the World in Climate Change Commitments”. Press Release, UK Government, Nov 2021.
- “AstraZeneca’s ‘Ambition Zero Carbon’ Strategy to Eliminate Emissions by 2025 and be Carbon Negative Across the Entire Value Chain by 2030”. Press Release, AstraZeneca, Jan 2020.
- “Chiesi Group Calls for #ActionOverWords in the Fight Against Climate Change”. Press Release, Chiesi, May 2021.
- Robinson J, “Chiesi Launches Postal Asthma Inhaler Recycling Scheme”. Pharm J, Feb 2021.
- Kunkel G et al, “Respimat (a New Soft Mist Inhaler) Delivering Fenoterol Plus Ipratropium Bromide Provides Equivalent Bronchodilation at Half the Cumulative Dose Compared with a Conventional Metered Dose Inhaler in Asthmatic Patients”. Respiration, 2000, Vol 63(7), pp 306–314.
- “Biologics Market – Growth, Trends, COVID-19 Impact, And Forecasts (2022–2027)”. Mordor Intelligence, 2021.
- “Data Privacy: What the Consumer Really Thinks”. Data & Marketing Association, Feb 2018.
- “Test Beds Programme – Information to Support the Launch of Wave 2”. NHS England, Mar 2018.
- “Global Inhalation and Nasal Sprays Generic Drugs Market Insights, Forecast to 2028”. QYResearch, Jan 2022.
- Beckman S, “Patients Prefer Epinephrine Nasal Spray Over Auto-Injector”. Healio, Nov 2019.
- “Injection Phobia”. Anxiety UK web page, accessed Mar 2022.
- An X et al, “Single-dose Intranasal Vaccination Elicits Systemic and Mucosal Immunity Against SARS-CoV-2”. iScience, 2021, Vol 24(9), Article 013037.

