Citation: Hopkins J, “How Digital Medical Devices are Meeting the Challenges of Clinical Trials”. ONdrugDelivery, Issue 121 (Jun 2021), pp 50–53.
Josh Hopkins discusses the challenges that have been present in conducting clinical trials at a central brick-and-mortar location since their inception, and how modern digitisation presents an opportunity to improve clinical trial methodology by liberating it from the need for an in-person central study site via the use of digital medical devices and technologies.
The Internet of Things (IoT) – defined simply as a system of internet-connected devices that collect and transfer data over a wireless network – has transformed healthcare, from electronic health records and patient portals to telemedicine. The introduction of next-generation 5G wireless technology in 2019 is serving to further advance the vast potential of digital health technology.
“Clinical trials are a complex process, from site selection and patient enrolment to study monitoring and data management. Digital health technology, with its connected ecosystem of applications and devices, presents a clear opportunity to improve data management in the clinical trial process.”
UNDERSTANDING DIGITAL HEALTH
The broad scope of digital health includes categories such as mobile health, health information technology, wearable devices, telehealth and telemedicine. Using computing platforms, connectivity, software and sensors, digital health technology creates opportunities for healthcare providers (HCPs) and other stakeholders to improve medical outcomes for patients and enhance the efficacy of treatments.
These technologies span a wide range of uses, from applications in general wellness to applications in the medical device sector. They include technologies intended for use as a medical product, in a medical product, as companion diagnostics or as an adjunct to other medical products (devices, drugs and biologics). They may also be used to develop or study medical products.1
Digital Medical Devices
Connected devices, such as smart insulin pens, connected inhalers and asthma monitors, empower patients to better manage their own health and access help quickly if something goes wrong. These devices also allow HCPs to monitor ongoing conditions and gather data remotely, allowing for observation and treatment that was previously only possible in an institutional setting.2
Consider respiratory conditions, such as asthma, where a lack of adherence to prescribed medication and insufficient disease monitoring can lead to uncontrolled or exacerbated health problems. Connected inhalers can track medication use, provide audio and visual alerts to remind patients to take a dose, and offer guidance to improve their inhaler technique and adherence to a medication plan, all leading to better management of the patient’s condition.
Aptar Pharma is a major player in this space and offers a broad range of digital healthcare solutions for the prevention, diagnosis and treatment of diseases, as well as patient monitoring and health management. Its wide range of connected devices, including in injectable and nasal drug delivery, is patient friendly, intuitive to use and supported by training devices from Noble, an Aptar Pharma company, that are developed and designed to replicate the real device experience.
“Sponsors, such as Sanofi and Pfizer, are aligning their business development strategies and designing new apps and wearables that not only enhance the collection of data, but also improve direct communication with patients, making it possible to adjust their studies on a timely basis.”
DIGITAL HEALTH TECHNOLOGY AND CLINICAL TRIALS
Clinical trials are essential for evaluating the safety and efficacy of new drugs, medical devices and other health system interventions. Clinical trials are a complex process, from site selection and patient enrolment to study monitoring and data management. Digital health technology, with its connected ecosystem of applications and devices, presents a clear opportunity to improve data management in the clinical trial process.
The Challenges of Current Clinical Trial Methods
In 1943, the first modern clinical trial for treatment of the common cold was conducted in the UK. Over 1,000 patients participated in the double-blind trial, whereby neither patients nor doctors knew what treatments were being given to which patients until the clinical trial was complete. Each patient travelled an average of two to three hours to reach a single, centralised trial location. The observations by clinical investigators were written by hand, and it took 18 months to synthesise the results and generate a report.3
Nearly eight decades later, traditional clinical trials remain cumbersome and labour intensive. Biotechnology companies must still recruit large numbers of patients to get the correct, statistically significant sample size, and most trial participants still have to go to brick-and-mortar research centres to receive treatment, often recording their symptoms and side effects on paper forms.
These operational inefficiencies inflate costs, increase participant burden and extend already lengthy clinical trial timelines. In addition, for patients who do not live close to a research site or who have mobility or scheduling constraints, participation can be expensive, or even impossible, thus increasing disparities in access to research and limiting the diversity of participants in a trial.4
Compounding these problems, the covid-19 pandemic has caused more than 1,000 clinical trials to be put on hold due to the risk of the virus spreading among trial participants, other nearby patients and healthcare workers.5 Nonetheless, more than half (54%) of surveyed device and diagnostics industry professionals anticipate a full recovery of clinical study activity before the end of 2021.6
One way to address these challenges lies in transforming the traditional clinical trial approach via the adoption of innovative new digital technologies to improve recruitment, patient retention, data collection and analytics.
The Future of Clinical Trials in the Digital Age
As the world progresses toward a more digitised future, sponsors involved in clinical trials reference four main benefits of adopting digital technology:7
- Cost reduction by 50% per participant compared with current onsite clinical trial methods
- Increased recruitment rate and diversification by making trial participation more convenient
- Increased data collection from participants, since longer time spans can be monitored
- Increased data quality based on participants’ natural environment instead of data collected by survey at the trial site.
Sponsors, such as Sanofi and Pfizer, are aligning their business development strategies and designing new apps and wearables that not only enhance the collection of data, but also improve direct communication with patients, making it possible to adjust their studies on a timely basis.
Another emerging innovative strategy is patient centricity. This approach puts the focus of clinical trials on the patient, in order to better respond to their needs and ensure their commitment throughout the clinical process.7
The Role of Connected Medical Devices
Connected medical devices and other digital technologies are playing a growing role in clinical research, with important implications for stakeholders across the entire research ecosystem. In both 2017 and 2018, over 1,100 unique trials included use of a connected digital product – a tenfold increase since the early 2000s.8
For pharmaceutical manufacturers and contract research organisations (CROs), the emergence of connected digital products into the clinical research space presents an opportunity to include novel trial endpoints that use real-world evidence. For patients, connected digital products can reduce the burden of trial participation and increase inclusivity by fostering remote monitoring and encouraging the enrolment of individuals who might not otherwise be able to participate due to socioeconomic circumstances or travel limitations.8
NOBLE SOLUTIONS SUPPORT THE ADOPTION OF DIGITAL MEDICAL DEVICES IN CLINICAL TRIALS
The medical device industry shares common regulations and guidance with the pharmaceutical industry. However, differences can exist relative to the design and management of clinical studies. Having the right partners is important for the adoption of digital medical devices in clinical trials.
Noble is one such partner. An industry leader in providing drug delivery training device programmes for pharmaceutical companies and original equipment manufacturers, Noble manufactures training devices for autoinjectors, injectable prefilled syringes, on-body systems and respiratory devices for patients who self-administer their prescribed drug therapies.
According to the European clinical research organisation ZAK-Pharma, as many as 85% of clinical trials fail to recruit and retain enough patients to meet their enrolment timeline.9 Alongside Aptar Pharma, Noble is developing connected training solutions that provide a more patient-centric experience and can support the digital transformation of clinical trials.
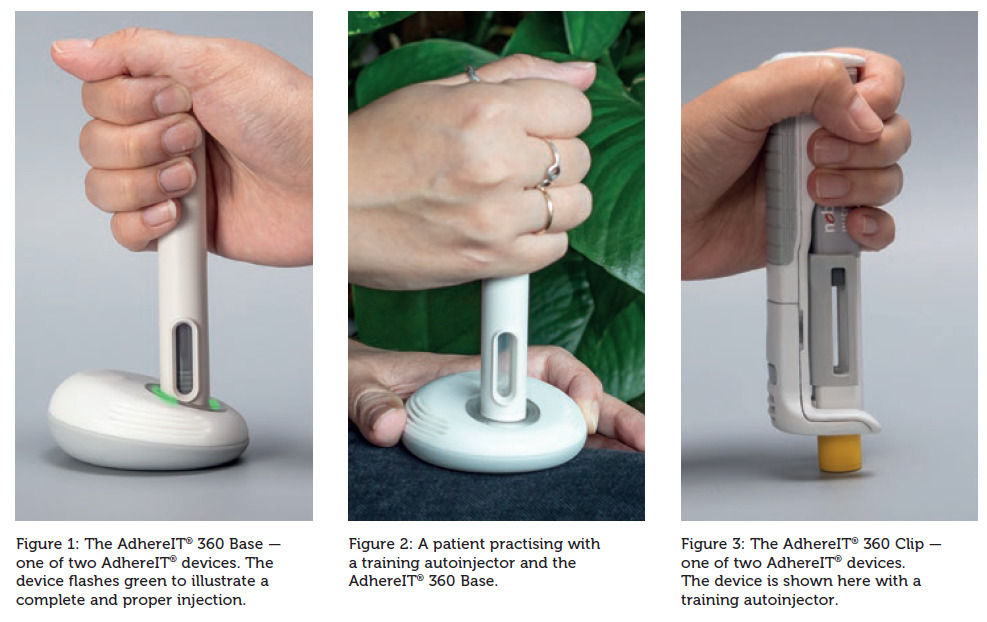
“Over the last year, we have seen an acceleration in pharma companies choosing to perform remote clinical trials,” states Adam Shain, Director, Digital Healthcare at Aptar Pharma. “Having a real-time mechanism with both devices and apps to ensure patients are utilising their medication correctly is critical for the success of any self-administered clinical trial. Partnered with Aptar’s digital ecosystem, Noble and Aptar Pharma’s AdhereIT® – a connected device that uses Bluetooth technology to pair autoinjectors with a software application to provide real-time feedback, both through the device and through the paired app, about whether a patient’s injection was performed correctly – plays a critical role in overcoming these challenges.”
“Another way Noble is contributing to streamlining and digitising clinical trials is with “Human Factors +”, an expanded service that combines human factors engineering with Noble’s robust training solutions.”
Tracking, Monitoring and Guiding Patients to Improved Adherence
As mentioned, one such example of a connected device used to monitor patient self-injection adherence is Noble and Aptar Pharma’s connected device, AdhereIT® (Figures 1–3). In addition to adherence monitoring, both the device itself and the app give patients feedback about whether a proper injection was performed. AdhereIT®’s training platform also includes a dashboard for HCPs to monitor patients’ therapeutic performance and provides biopharmaceutical companies with valuable non-patient-specific adherence behaviour information.
“Connected medical devices represent the future of healthcare for patients, pharmaceutical companies and HCPs, playing a vital role in the remote tracking and treatment of chronic illnesses and delivering a range of benefits that include improved drug management, enriched patient experiences and enhanced patient outcomes,” said Tim McLeroy, Noble’s executive director of marketing and patient services. “The connectivity of digital technology solutions like AdhereIT® also creates market differentiation and enables value-based contracting for biopharmaceutical companies and medical device manufacturers to survive in a competitive and challenging marketplace.”
Empirical and Analytical Evidence with Human Factors Engineering
Another way Noble is contributing to streamlining and digitising clinical trials is with “Human Factors +” (HF+), an expanded service that combines human factors engineering with Noble’s robust training solutions. By doing so, Noble helps advance the development and testing of new self-administered medical products that optimise efficacy and safety while minimising use errors and the risk of adverse events.
“Human factors engineering provides empirical and analytical evidence that a device and its labelling can be used safely and effectively by the intended patient,” said Kevin Cluff, PhD, Noble’s acting director of human factors. “The process involves testing the numerous touchpoints where patients interface with a drug product, including packaging, instructions for use (IFUs), prescribing information, quick reference guides and device indicators and controls.”
Noble’s HF+ capabilities complement the company’s expertise in the areas of conceptualisation, design and development, mechanical/electrical/software engineering, project management, quality management, manufacturing, commercialisation and logistics services.
Meeting the Challenges of Clinical Trials
Noble’s connected medical device solutions and other services offer the following benefits to meet the challenges of clinical trials:
- Reduction of timelines due to increased speed-to-market
- Reduction of false positives
- Reduction of dropouts due to noncompliance
- Remote patient monitoring
- Assurance that a complete dose has been given
- Identification of medication errors
- Capture of date and time of injection
- Easy and quick capture and aggregation of data
- Minimisation of the need for live visits and travel
- Decentralisation of study
- Patients are active stakeholders rather than passive participants.
CONCLUSION
Harnessing the digital convergence of people, information, technology and connectivity offers real opportunities to improve clinical trials. Digital medical devices can help meet the challenges of today’s arduous clinical trials, providing a better patient experience and more holistic view of a patient’s health, thus enabling remote patient monitoring and enhancing the quality, quantity and frequency of data collection during clinical trials and with connected devices in the real world.
REFERENCES
- “What is Digital Health?”. US FDA, web page.
- Sentance R, “7 examples of how the internet of things is facilitating healthcare”. Econsultancy, Jan 2021.
- Kudumala A et al, “Reimagining clinical trials in the age of the digital patient”. Deloitte, 2019.
- Inan OT et al, “Digitizing clinical trials”. npj Digit Med, 2020, Vol 3, article 101.
- Ripton JT, “Decentralized clinical trials are opening the drug development pipeline”. MedCity News, Mar 2021.
- “Modernizing Clinical Research: Keeping Pace with Medical Device & Diagnostics Innovation”. MassDevice, Oct 2020.
- Brucher L et al, “Digitalization of clinical trials. How new technologies enhance the future of healthcare”. Inside Magazine, Nov 2018, Issue 19, pp 98–101.
- Marra C et al, “Quantifying the use of connected digital products in clinical research”. njp Digit Med, 2020, Vol 3, article 50.
- Rutter A, “7 Reasons your Clinical Trial isn’t recruiting enough patients”. ZAK-Pharma, Aug 2019.

