To Issue 154
Citation: Heraghty F, Jameson H, “The End of the Road for pMDIs?”. ONdrugDelivery, Issue 154 (Nov 2023), pp 22–26.
Finn Heraghty and Heather Jameson explore the extent to which the healthcare needs of a population could be covered by the combined use of soft mist inhalers and dry powder inhalers, and discuss the factors that will impact the continued importance of pressurised metered dose inhalers going forward.
“The main challenge to the ongoing dominance of pMDIs is the GWP of their current propellants.”
For decades, the portable inhaler market has been dominated by two categories of inhaler – pressurised metered dose inhalers (pMDIs) and dry powder inhalers (DPIs). In recent years, other categories have emerged, such as soft mist inhalers (SMIs).
At the moment, pMDIs still make up the majority of inhalers purchased by the UK NHS. However, considering the impending transition away from high global warming potential (GWP) propellants, such as hydrofluoroalkanes (HFAs), that pMDIs currently use, how long will this remain the case? The Swedish market, where pMDIs make up only 10% of inhalers, provides evidence that heavy reliance on pMDIs is not essential to meet the healthcare needs of a population. Might we be approaching the end of the road for pMDIs?
pDMIs AND THEIR EVOLUTION
Since their introduction in the 1950s, pMDIs have been a mainstay in respiratory therapy.1 A key advantage of pMDIs has always been their low cost. The drug is stored at high pressure in a canister in solution or suspension with the propellant(s), and aerosolisation is achieved by releasing the high-pressure propellant through a nozzle.
This method has proven effective in managing respiratory conditions, but is not without its drawbacks. For example, some patients may find it difficult to co-ordinate their inhalation with the release of the medication, potentially leading to suboptimal dosing. Some breath-activated pMDIs have been introduced to help resolve this issue, but these come with increased complexity, and therefore increased cost. Furthermore, the relatively fast spray velocity tends to result in a higher than ideal deposition of aerosol particles onto the back of the throat rather than into the deep lung. Use of a spacer (as shown in Figure 1) improves these issues, but they are bulky and so are often neglected, particularly when not at home or in hospital.

Figure 1: A pMDI used with a spacer can improve ease of use.
The main challenge to the ongoing dominance of pMDIs is the GWP of their current propellants.2 Originally, chlorofluorocarbons (CFCs) were used in pMDIs, which are not only potent greenhouse gases, but also found to be ozone depleting.3 After the introduction of the Montreal Protocol in 1987, which was designed to regulate the use of ozone-depleting chemicals, a transition was made to using hydrofluoroalkanes (HFAs) instead. However, although these are not known to harm the ozone layer, they are still potent greenhouse gases – the use of which vastly outweighs any environmental impact due to the materials used in the manufacture of the device itself.2 The Kigali Amendment to the Montreal Protocol aims to reduce global HFA consumption by 80% by 2047,4 with the even stricter requirement to do so in the EU by 2030.5
It is clear that we are approaching a turning point for pMDIs. The question is – will HFA-powered pMDIs be replaced by lower-GWP propellants or by different devices?
“Researchers and pharmaceutical companies are already actively searching for alternative propellants to replace the current options.”
NEXT-GENERATION PROPELLANTS
Researchers and pharmaceutical companies are already actively searching for alternative propellants to replace the current options. Table 1 summarises some of the main lower-GWP candidates currently being considered, compared with some of those that are currently in use.6
| Propellant | Current or New |
GWP (CO2 = 1) |
Comments |
| 1,1,1,2,3,3,3-Heptafluoropropane (HFC-227ea) |
Current | 3220 | High GWP |
| 1,1,1,2-Tetrafluoroethane (HFC-134a) |
Current (majority) | 1430 | High GWP |
| 1,1-Difluoroethane (HFA-152a) |
New | 124 | Flammability concerns Moderate GWP |
| 1,3,3,3-Tetrafluoropropene (HFO-1234ze(E)) |
New | <1 | Low GWP Could be banned in EU under REACH PFAS regulations, status should be clarified in 2024 |
Table 1: Summary of pMDI propellants.
Concerns remain around the new propellants proposed; there are flammability concerns for HFA-152a, particularly during manufacture and processing of the drug product,5 and there is a risk that HFO-1234ze(E) could be banned under European REACH PFAS regulations7 – the status of which should be clarified in 2024. The design of pMDI nozzles will also need to be optimised to work effectively with the new propellant(s) to compensate for the different physical properties.
Challenging timelines face pDMIs to meet the HFA restriction deadlines. New formulations will need to be brought to market in the next few years in optimised actuators with low-GWP propellants, and these propellants will need to be available at commercially viable prices with the quality and security of supply required for drug delivery devices. While pMDIs powered by low-GWP propellants may prove to be technically viable, market pressures may lead to a shift towards a greater market share of alternative devices.
DPIs: A PROVEN ALTERNATIVE?
DPIs have gained popularity as an alternative to pMDIs, first being introduced slightly later than pMDIs in 1967.8 Unlike pMDIs, DPIs deliver medication in a fine powder form that does not require a propellant, therefore eliminating the concerns regarding greenhouse gas emissions from use.
DPIs can effectively treat a similar range of respiratory conditions to pMDIs, provided the medication can be formulated as a dry powder. The powder is often stored in sealed capsules (Figure 2) to prevent contact with moisture, which could interfere with the ability of the powder to disperse effectively.
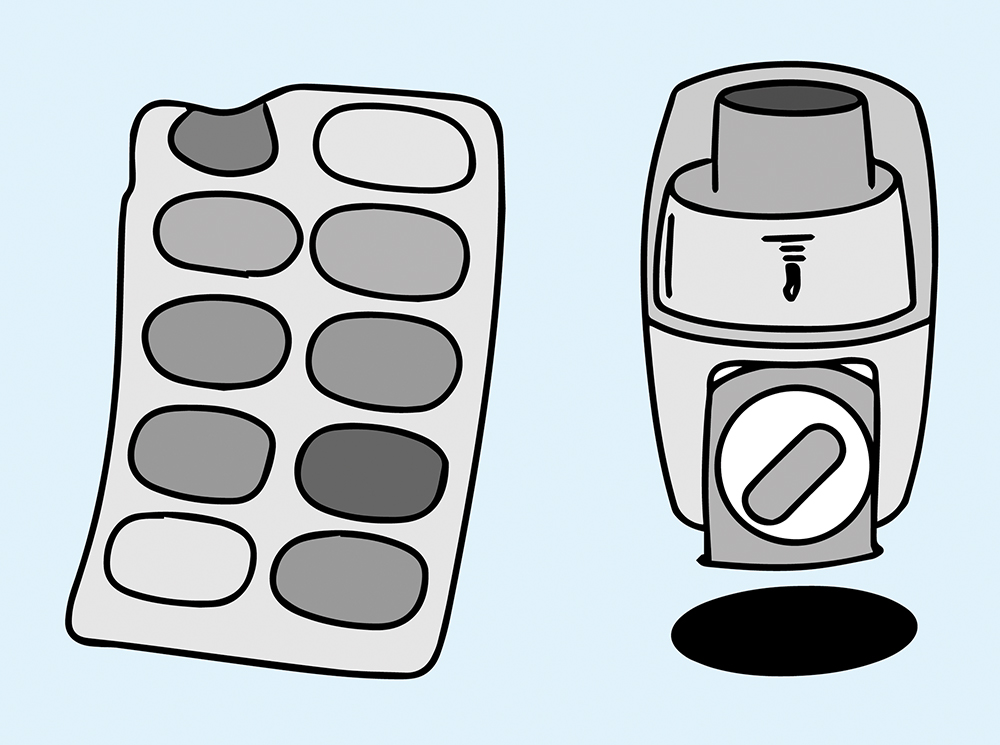
Figure 2: A common DPI format – capsules of dry powder (left) alongside the device (right).
The Swedish healthcare model is often quoted as an example success story for the DPI – in 2011 approximately 90% of inhaler devices sold and used in Sweden were DPIs whereas, in the UK, approximately 80% were pMDIs.9 This demonstrates that it should be theoretically possible to provide for the healthcare needs of a population with a lower reliance on pMDIs. However, there are practical reasons why healthcare services in countries such as the UK and the US have a preference for pMDIs over DPIs.
Economic Pressures
A key reason for the widespread use of pMDIs is their low cost per unit. Analysis presented in 2019 assessed the potential cost to the NHS of a wholesale switch from using pMDIs (currently pMDIs account for approximately 80% of inhaler devices) to DPIs.10 The study concluded that there would be a £127 million rise in prescribing costs per annum, representing around an additional 10% cost of respiratory therapy. The estimate was dependant on the ratio of branded products to generics employed, and it was suggested that a cost saving could be made if only generic DPIs were used.
However, given the investment that will be needed to transition pMDIs to new propellants, it is to be expected that their unit cost may increase, reducing the perceived benefit of pMDIs over DPIs.
Usability Concerns
DPIs work by relying on the patient’s own inhalation to disperse and deliver the powdered medication into the lungs, which ensures that the medication is released only when the patient inhales correctly. This eases the need for careful co-ordination compared with pMDIs but, conversely, the sharp intake of breath required may not be possible for some patients, particularly those with the types of chronic lung conditions often treated with inhaled medications. Hence, there may be a subset of a population for which DPIs are simply not suitable – such as children, the elderly and those with severe respiratory conditions. This could mean there is an ongoing need for pMDIs for some users, even if diminished – unless alternative options could cover this gap?
SMIs: A GENTLE APPROACH
SMIs have been a recent and successful addition to the suite of available inhaler options, with the Boehringer Ingelheim Respimat being the first SMI, marketed in 2004.8 As Spiriva (Boehringer Ingelheim), a successful drug for the treatment of chronic obstructive pulmonary disease (COPD), is also beginning to come off-patent across the globe, several companies have designs for generic alternatives in the pipeline, from Merxin to invoX Pharma, previously Softhale (Diepenbeek, Belgium),11 and we should expect other novel soft mist device platforms to follow.
SMIs generally work by forcing liquid through one or more small nozzles to generate a fine aerosol mist, although different mechanisms have been explored, including impinging jets (Respimat – Figure 3) and Rayleigh break-up (Medspray). A spring or other mechanical system is used to generate the required pressure instead of a propellant, thereby also removing the issue of emissions from use.

Figure 3: The fine mist produced by the Respimat SMI.
The aerosolised drug solutions are expelled in a slow-moving jet, which reduces undesired oropharyngeal deposition and makes it much easier to successfully perform the sequence between actuation and inhalation11 compared with a pMDI. The aerosol fine-droplet fraction from the Respimat is reported to be approximately double that of a pMDI,12 meaning half the dose with a Respimat is able to achieve the same therapeutic outcome as the full dose administered by pMDI. The soft mist delivery format is also well suited for patients who struggle with generating the required inspiratory force for DPIs.
However, SMIs are not suitable in all applications. As the medication is typically forced through a very small nozzle (sometimes less than 5 μm), current technologies cannot be used with drugs in suspension, as the particles could either block the nozzle or be filtered out in the filter typically employed upstream of the nozzle. SMIs are also currently significantly more complex and expensive than pMDIs, but there is active interest in the market to identify new, simpler soft-mist mechanisms, with the goal of bringing the cost per unit closer to that of pMDIs. If this could be realised, the usability benefits of the SMI will provide strong competition to the pMDI.
“When considering the delivery of biologics via oral inhalation, discussion of devices generally focuses on the varying merits and demerits of DPIs, nebulisers and SMIs – neglecting pMDIs.”
FUTURE PHARMACEUTICAL TRENDS – BIOLOGIC DELIVERY
There has been growing interest in recent years about the potential advantages of delivering biologic drugs via inhalation.13 The inhalation route is non-invasive and suitable for both local and systemic delivery, and inhalers have advantages for unassisted use in non-clinical environments.
When considering the delivery of biologics via oral inhalation, discussion of devices generally focuses on the varying merits and demerits of DPIs, nebulisers and SMIs – neglecting pMDIs. The inherent temperatures and pressures involved in delivery and the risk of denaturing on aerosolisation14 means pMDIs are not easily compatible with biologic drugs. There is concern over the interaction between the propellant used in pMDIs and the biologics, which can lead to the denaturing of proteins and peptides.15 Poor solubility of biologics in the propellants also limits the dose range that can be delivered per actuation.16 This is a growing market sector where pMDIs appear to be being left behind – a further indicator that their days may be numbered (Table 2).
| Device Type |
Reasons to Expect Continued or Growing Use |
Barriers to Growth |
| pMDI |
|
|
| DPI |
|
|
| SMI |
|
|
Table 2: Summary of advantages and disadvantages for different inhaler options.
CONCLUSION
So, are the next few years the end of the road for pMDIs? They will have a future if new formulations can be brought to market in the next few years in optimised actuators with low-GWP propellants that:
- Have acceptable flammability (a concern for HFA–152a)
- Meet PFAS regulations (a concern for HFO–1234ze)
- Are available at commercially viable prices with the quality and security of supply required for drug delivery devices.
However, if those criteria are not met, then we should expect DPIs and SMIs to take an increasing market share in all markets in the years to come.
REFERENCES
- Crompton G, “A brief history of inhaled asthma therapy over the last fifty years”. Prim Care Respir J, 2006, Vol 15(6), pp 326–331.
- Udale R, Eldridge C, Shah O, “Are Governments Banning the Most Environmentally Friendly Inhaler?”. ONdrugDelivery, Issue 132 (Apr–May 2022), pp 30–35.
- Wilkinson AJK, Braggins R, Steinbach I et al, “Costs of switching to low global warming potential inhalers. An economic and carbon footprint analysis of NHS prescription data in England”. BMJ Open 2019, Vol 9(10), Article 028763.
- “UK Progress on reducing F-gas Emissions”. House of Commons Environmental Audit Committee, Apr 25, 2018F.
- Parry M, “Considerations when Switching from Current pMDI Propellants to New Lower-GWP Propellants”. ONdrugDelivery, Issue 145 (Apr 2023), pp 6–9.
- “Tackling a changing climate; Metered dose inhalers”. Recipharm, Apr 25, 2018.
- “PFAS refrigerant ban could impact EU green aims”. Cooling Post, Jan 4, 2023.
- Stein SW, Thiel CG, “The History of Therapeutic Aerosols: A Chronological Review”. JAerosol Med Pulm Drug Deliv, 2017, Vol 30(1), pp 20–41.
- Lavorini F, Corrigan CJ, Barnes PJ et al, “Retail sales of inhalation devices in European countries: so much for a global policy”. Respir Med, 2011, Vol 105(7), pp 1099–103.
- Wilkinson AJK et al, “Costs of switching to low global warming potential inhalers. An economic and carbon footprint analysis of NHS prescription data in England”. BMJ Open, 2019, Vol 9(10), Article 028763.
- Udale R, Jameson H, “Waiting with Bated Breath – What’s in Store for 2022”. ONdrugDelivery, Issue 131 (Apr 2022), pp 6–9.
- Kunkel G, Magnussen H, Bergmann K et al, “Respimat (a new soft mist inhaler) delivering fenoterol plus ipratropium bromide provides equivalent bronchodilation at half the cumulative dose compared with a conventional metered dose inhaler in asthmatic patients”. Respiration, 2000, Vol 67(3), pp 306–314.
- Gonda I, “Is There a Future for the Respiratory Delivery of Biologics?”. ONdrugDelivery, Issue 96 (Apr 2019), pp 6–10.
- Moore S, Harper K, Marshall S, “Key Considerations for Non-Clinical Safety Assessment of Inhaled Biopharmaceuticals”. ONdrugDelivery, Issue 80 (Nov 2017), pp 46–49.
- Agu R et al, “The lung as a route for systemic delivery of therapeutic proteins and peptides”. Respir Res, 2001, Vol 2, pp 198–209.
- Fathe K et al, “Inhaled Biologics: From Preclinical to Product Approval”. Curr Pharm Des, 2016, Vol 22, pp 2501–2521.

